Abstract
Background
The development of atrial fibrillation (AF) during the course of acute coronary syndrome (ACS) is related to poor prognosis. Possible predictors of new-onset AF (NOAF) have not been adequately investigated in elderly patients with ACS undergoing percutaneous coronary intervention (PCI). We aimed to identify the factors associated with NOAF in such patients.
Methods
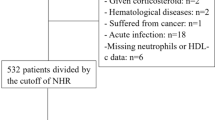
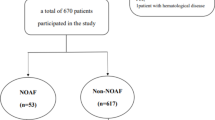
A total of 308 elderly patients with ACS undergoing PCI were enrolled in the study. Patients were divided into two groups: without NOAF [254 patients, 64.6% men, age: 73.5 (69.0–79.0) years] and with NOAF [54 patients, 70.4% men, age: 75.0 (68.7–81.2) years]. Clinical, angiographic, and laboratory features including neutrophil-to-lymphocyte ratio (NLR) and monocyte-to-high-density lipoprotein ratio (MHR) were compared between the groups.
Results
The percentages of prior myocardial infarction (MI) (20.4 vs. 5.9%) and Killip III/ IV (24.1 vs. 7.1%), NLR [4.5 (2.6–7.2) vs. 3.2 (2.0–6.0)], and MHR [19.4 (15.7–26.5) vs. 12.9 (9.9–18.5)] were higher in patients with NOAF compared to the others (p = 0.020, < 0.001, 0.030, and < 0.001, respectively). In multivariate regression analysis, prior MI (OR 4.509, 95% CI 1.679–12.106, p = 0.003) and MHR (OR 1.102, 95% CI 1.054–1.152, p < 0.001) independently predicted NOAF. In addition, Killip III/IV was found to be an independent predictor of 6-month overall mortality (HR 2.949, 95% CI 1.218–7.136, p = 0.016).
Conclusions
Prior MI and MHR are independent predictors of NOAF in elderly patients with ACS undergoing PCI. Killip III/IV predicts 6-month overall mortality in such patients.

Similar content being viewed by others
References
O’Gara PT, Kushner FG, Ascheim DD et al (2013) 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 61:e78–e140
Amsterdam EA, Wenger NK, Brindis RG et al (2014) 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 64:e139–e228
Vandecasteele EH, De Buyzere M, Gevaert S et al (2013) Reperfusion therapy and mortality in octogenarian STEMI patients: results from the Belgian STEMI registry. Clin Res Cardiol 102:837–845
Wang J, Yang YM, Zhu J (2015) Mechanisms of new-onset atrial fibrillation complicating acute coronary syndrome. Herz 40:18–26
Schmitt J, Duray G, Gersh BJ et al (2009) Atrial fibrillation in acute myocardial infarction: a systematic review of the incidence, clinical features and prognostic implications. Eur Heart J 30:1038–1045
Gorenek B, Blomström Lundqvist C, Brugada Terradellas J et al (2014) Cardiac arrhythmias in acute coronary syndromes: position paper from the joint EHRA, ACCA, and EAPCI task force. Europace 16:1655–1673
Jabre P, Jouven X, Adnet F et al (2011) Atrial fibrillation and death after myocardial infarction: a community study. Circulation 123:2094–2100
Kaya MG, Akpek M, Lam YY et al (2013) Prognostic value of neutrophil/lymphocyte ratio in patients with ST-elevated myocardial infarction undergoing primary coronary intervention: a prospective, multicenter study. Int J Cardiol 168:1154–1159
Cetin MS, Ozcan Cetin EH, Kalender E et al (2016) Monocyte to HDL cholesterol ratio predicts coronary artery disease severity and future major cardiovascular adverse events in acute coronary syndrome. Heart Lung Circ 25:1077–1086
Kurtul A, Yarlioglues M, Duran M (2017) Predictive value of CHA2DS2–VASC score for contrast-induced nephropathy after percutaneous coronary intervention for acute coronary syndrome. Am J Cardiol 119:819–825
Mehran R, Nikolsky E (2006) Contrast-induced nephropathy: definition, epidemiology, and patients at risk. Kidney Int Suppl 100:S11-S15
Levey AS, Bosch JP, Lewis JB et al (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130:461–470
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1–39
Mauri L, Hsieh WH, Massaro JM et al (2007) Stent thrombosis in randomized clinical trials of drug-eluting stents. N Engl J Med 356:1020–1029
Ruwald AC, Bloch Thomsen PE, Gang U et al (2013) New-onset atrial fibrillation predicts malignant arrhythmias in post-myocardial infarction patients—a Cardiac Arrhythmias and Risk Stratification after acute Myocardial infarction (CARISMA) substudy. Am Heart J 166:855–863
Chesebro JH, Knatterud G, Roberts R et al (1987) Thrombolysis in Myocardial Infarction (TIMI) Trial, phase I: a comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge. Circulation 76:142–154
Mrdovic I, Savic L, Krljanac G et al (2012) Incidence, predictors, and 30-day outcomes of new-onset atrial fibrillation after primary percutaneous coronary intervention: insight into the RISK-PCI trial. Coron Artery Dis 23:1–8
Crenshaw BS, Ward SR, Granger CB et al (1997) Atrial fibrillation in the setting of acute myocardial infarction: the GUSTO-I experience. Global utilization of streptokinase and TPA for occluded coronary arteries. J Am Coll Cardiol 30:406–413
Raposeiras Roubín S, Abellas-Sequeiros RA, Abu Assi E et al (2015) Relation of contrast induced nephropathy to new onset atrial fibrillation in acute coronary syndrome. Am J Cardiol 115:587–591
Annoura M, Ogawa M, Kumagai K et al (1999) Cholesterol paradox in patients with paroxysmal atrial fibrillation. Cardiology 92:21–27
van der Wal AC, Becker AE, van der Loos CM et al (1994) Site of intimal rupture or erosion of thrombosed coronary atherosclerotic plaques is characterized by an inflammatory process irrespective of the dominant plaque morphology. Circulation 89:36–44
Guo Y, Lip GY, Apostolakis S (2012) Inflammation in atrial fibrillation. J Am Coll Cardiol 60:2263–2270
Karataş MB, Çanga Y, İpek G et al (2016) Association of admission serum laboratory parameters with new-onset atrial fibrillation after a primary percutaneous coronary intervention. Coron Artery Dis 27:128–134
Chavarria N, Wong C, Hussain H et al (2015) Persistent elevation of neutrophil/lymphocyte ratio associated with new onset atrial fibrillation following percutaneous coronary intervention for acute ST segment elevation myocardial infarction. J Ayub Med Coll Abbottabad 27:441–447
Mestas J, Ley K (2008) Monocyte-endothelial cell interactions in the development of atherosclerosis. Trends Cardiovasc Med 18:228–232
Woollard KJ, Geissmann F (2010) Monocytes in atherosclerosis: subsets and functions. Nat Rev Cardiol 7:77–86
Murphy AJ, Woollard KJ (2010) High-density lipoprotein: a potent inhibitor of inflammation. Clin Exp Pharmacol Physiol 37:710–718
Wasilewski J, Desperak P, Hawranek M et al (2016) Prognostic implications of mean platelet volume on short- and long-term outcomes among patients with non-ST-segment elevation myocardial infarction treated with percutaneous coronary intervention: a single-center large observational study. Platelets 27:452–458
Acknowledgements
We are grateful for the assistances from Mehmet Eren Altınbaş, Özlem Karabulut, Nurcan Göküz and Sinem Tekin.
Funding
No financial support from any organization was used in the preparation of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no competing interests.
Ethical approval
The study was approved by the Ethics Committee of Eskisehir Osmangazi University, Faculty of Medicine. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
All patients were informed about the nature of the study and a written informed consent was obtained.
Rights and permissions
About this article
Cite this article
Ulus, T., Isgandarov, K., Yilmaz, A.S. et al. Predictors of new-onset atrial fibrillation in elderly patients with acute coronary syndrome undergoing percutaneous coronary intervention. Aging Clin Exp Res 30, 1475–1482 (2018). https://doi.org/10.1007/s40520-018-0926-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-018-0926-9