Abstract
Introduction
“Giving or receiving a patient handover to transition patient care responsibility” is one of the thirteen Core Entrustable Professional Activities (Core EPAs) for Entering Residency. However, implementing a patient handover curriculum in undergraduate medical education (UME) remains challenging. Educational leaders in the multi-institutional Core EPA8 pilot workgroup developed a longitudinal patient handover UME curriculum that was implemented at two pilot institutions.
Materials and Methods
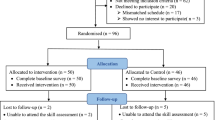
We utilized multi-school graduation questionnaire data to assess the association of our patient handover curriculum on self-reported frequency of observation/feedback and skill acquisition by comparing data from the shared curriculum schools to data from other Core EPA pilot schools (three schools with school-specific curriculum; five without a dedicated handover curriculum). Questionnaire data from 1,278 graduating medical students of the class of 2020 from all ten Core EPA pilot schools were analyzed.
Results
Graduates from the two medical schools that implemented the shared patient handover curriculum reported significantly greater frequency of handover observation/feedback compared to graduates at the other schools (school-specific curriculum (p < .05) and those without a handover curriculum (p < .05)). Graduates from the two shared approach schools also more strongly agreed that they possessed the skill to perform handovers compared to graduates from the other eight pilot schools that did not implement this curriculum.
Conclusion
The findings of this study suggest that the implementation of a multi-institutional Core EPA–based curricular model for teaching and assessing patient handovers was successful and could be implemented at other UME institutions.


Similar content being viewed by others
References
Englander R, Flynn T, Call S, et al. Toward defining the foundation of the MD degree: core entrustable professional activities for entering residency. AcadMed. 2016;91(10):1352–8. https://doi.org/10.1097/ACM.0000000000001204.
O’Toole J, Calaman S, Everhart J, et al. I-PASS handoff curriculum: medical student workshop. MedEdPORTAL. 2014;(10). https://doi.org/10.15766/mep_2374-8265.9854.
Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803–12. https://doi.org/10.1056/NEJMsa1405556.
Reyes J, Greenberg L, Lesky L. ACCEPT medical student handoff workshop: the patient safety curriculum starts in undergraduate medical education. MedEdPORTAL. 2015;11. https://doi.org/10.15766/mep_2374-8265.10302.
Davis J, Roach C, Elliott C, Mardis M, Justice EM, Riesenberg LA. Feedback and assessment tools for handoffs: a systematic review. J Grad Med Educ. 2017;9(1):18–32. https://doi.org/10.4300/JGME-D-16-00168.1.
Liston BW, Tartaglia KM, Evans D, Walker C, Torre D. Handoff practices in undergraduate medical education. J Gen Intern Med. 2014;29(5):765–9. https://doi.org/10.1007/s11606-014-2806-0.
Gordon M, Hill E, Stojan JN, Daniel M. Educational interventions to improve handover in health care: an updated systematic review. Acad Med. 2018;93(8):1234–44. https://doi.org/10.1097/ACM.0000000000002236.
Sheng J, Manjunath S, Michael M, Gajera P, Wang E, Sendelbach D, et al. Integrating handover curricula in medical school. Clin Teach. 2020;17:661–8.
Chu ES, Reid M, Burden M, et al. Effectiveness of a course designed to teach handoffs to medical students. J Hosp Med. 2010;5(6):344–8. https://doi.org/10.1002/jhm.633.
Darbyshire D, Gordon M, Baker P. Teaching handover of care to medical students. Clin Teach. 2013;10(1):32–7. https://doi.org/10.1111/j.1743-498X.2012.00610.x.
O’Toole JK, Stevenson AT, Good BP, et al. Closing the gap: a needs assessment of medical students and handoff training. J Pediatr. 2013;162(5):887-888.e1. https://doi.org/10.1016/j.jpeds.2013.01.045.
Burns R, Nicholson A, Mangold K, Adler M, Trainor J. Pediatric boot camp series: assessment and plans, task prioritization, answering pages, handoffs. MedEdPORTAL. 2015;(11). https://doi.org/10.15766/mep_2374-8265.10310.
Reyes JA, Greenberg L, Amdur R, Gehring J, Lesky LG. Effect of handoff skills training for students during the medicine clerkship: a quasi-randomized study. Adv Health Sci Educ Theory Pract. 2016;21(1):163–73. https://doi.org/10.1007/s10459-015-9621-1.
Royce CS, Atkins KM, Mendiola M, Ricciotti H. Teaching patient handoffs to medical students in obstetrics and gynecology: simulation curriculum and assessment tool. MedEdPORTAL. 2016;12:10479. https://doi.org/10.15766/mep_2374-8265.10479.
Joyce AH. Team-based simulation for medical student handoff education. MedEdPORTAL. 2016;(12). https://doi.org/10.15766/mep_2374-8265.10486.
Davis R, Davis J, Berg K, et al. Patient handoff education: are medical schools catching up? Am J Med Qual. 2018;33(2):140–6. https://doi.org/10.1177/1062860617719128.
Thaeter L, Schröder H, Henze L, et al. Handover training for medical students: a controlled educational trial of a pilot curriculum in Germany. BMJ Open. 2018;8(9): e021202. https://doi.org/10.1136/bmjopen-2017-021202.
Arora VM, Eastment MC, Bethea ED, Farnan JM, Friedman ES. Participation and experience of third-year medical students in handoffs: time to sign out? J Gen Intern Med. 2013;28(8):994–8. https://doi.org/10.1007/s11606-012-2297-9.
Young JQ, Ten Cate O, O’Sullivan PS, Irby DM. Unpacking the complexity of patient handoffs through the lens of cognitive load theory. Teach Learn Med. 2016;28(1):88–96. https://doi.org/10.1080/10401334.2015.1107491.
Gaffney S, Farnan JM, Hirsch K, McGinty M, Arora VM. The modified, multi-patient observed simulated handoff experience (M-OSHE): assessment and feedback for entering residents on handoff performance. J Gen Intern Med. 2016;31(4):438–41. https://doi.org/10.1007/s11606-016-3591-8.
Bowen L, Marshall M, Murdoch-Eaton D. Medical student perceptions of feedback and feedback behaviors within the context of the educational alliance. Acad Med. 2017;92(9):1303–12. https://doi.org/10.1097/ACM.0000000000001632.
Murdoch-Eaton D, Bowen L. Feedback mapping - the curricular cornerstone of an educational alliance. Med Teach. 2017;39(5):540–7. https://doi.org/10.1080/0142159X.2017.1297892.
Core EPAs Guiding Principles. Association of American medical colleges. https://www.aamc.org/initiatives/coreepas/454358/guidingprincipleshomepage.html. Accessed 13 Feb 2019.
Association of American Medical Colleges. Core entrustable professional activities for entering residency: curriculum developers’ guide. AAMC iCollaborative. 2014:114. https://www.aamc.org/initiatives/coreepas/publicationsandpresentations/. Accessed 20 Oct 2018.
Kennedy TJ, Regehr G, Baker GR, Lingard L. Point-of-care assessment of medical trainee competence for independent clinical work. AcadMed. 2008;83(10 Suppl):S89-92. https://doi.org/10.1097/ACM.0b013e318183c8b7.
Aylward M, Nixon J, Gladding S. An entrustable professional activity (EPA) for handoffs as a model for EPA assessment development. Acad Med. 2014;89(10):1335–40. https://doi.org/10.1097/ACM.0000000000000317.
Starmer A, Landrigan C, Srivastava R, et al. I-PASS handoff curriculum: faculty observation tools. MedEdPORTAL. 2013;(9). https://doi.org/10.15766/mep_2374-8265.9570.
Association of American Medical Colleges. Medical School Graduation Questionnaire: 2020 all schools summary report. Association of American Medical Colleges. https://www.aamc.org/media/46851/download. Accessed 14 Feb 2022.
Bump GM, Jacob J, Abisse SS, Bost JE, Elnicki DM. Implementing faculty evaluation of written sign-out. Teach Learn Med. 2012;24(3):231–7. https://doi.org/10.1080/10401334.2012.692271.
Lupi CS, Ownby AR, Jokela JA, et al. Faculty development revisited: a systems-based view of stakeholder development to meet the demands of entrustable professional activity implementation. Acad Med. Published online May 22, 2018. https://doi.org/10.1097/ACM.0000000000002297.
Sedikides C. Assessment, enhancement, and verification determinants of the self-evaluation process. J Pers Soc Psychol. 1993;65(2):317–38. https://doi.org/10.1037/0022-3514.65.2.317.
Hynes H, Stoyanov S, Drachsler H, et al. Designing learning outcomes for handoff teaching of medical students using group concept mapping: findings from a multicountry European study. Acad Med. 2015;90(7):988–94. https://doi.org/10.1097/ACM.0000000000000642.
Obeso V, Brown D, Alyer M, et al. Toolkits for the 13 core entrustable professional activities for entering residency. Published online 2017. https://www.aamc.org/what-we-do/mission-areas/medical-education/cbme/core-epas/publications. Accessed 6 Jun 2019.
Chen HC, van den Broek WES, ten Cate O. The case for use of entrustable professional activities in undergraduate medical education. Acad Med. 2015;90(4):431. https://doi.org/10.1097/ACM.0000000000000586.
Rekman J, Hamstra SJ, Dudek N, Wood T, Seabrook C, Gofton W. A new instrument for assessing resident competence in surgical clinic: the Ottawa Clinic Assessment Tool. J Surg Educ. 2016;73(4):575–82. https://doi.org/10.1016/j.jsurg.2016.02.003.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
AAMC GQ wording on patient handover (EPA8) activities:
Indicate whether you agree or disagree with the following statements about your preparedness for beginning a residency program: I have the skills to “Give or receive a patient handover to transition care responsibility.”
AAMC GQ item: “In the workplace (clinical setting), how often during medical school have supervising residents or faculty members directly observed you performing the following activity and also provided you with immediate (within 24 h) verbal or written feedback on your performance of the activity? Include only activities involving real patients. Do NOT include activities involving standardized or simulated patients.” for the activity, “Give or receive a patient handover to transition care responsibility.”
Rights and permissions
About this article
Cite this article
Garber, A.M., Ownby, A.R., Trimble, G. et al. Evaluating the Association of a Core EPA–Oriented Patient Handover Curriculum on Medical Students’ Self-reported Frequency of Observation and Skill Acquisition. Med.Sci.Educ. 32, 855–864 (2022). https://doi.org/10.1007/s40670-022-01578-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-022-01578-x