Abstract
Purpose
A normal sagittal vertical axis (SVA) after spinal deformity correction can yield mechanical complications of up to 30%. Post-operative compensatory pelvic orientation can produce a normal SVA. We assess relative pelvic version (RPV), an individualised measure, for persistent post-operative compensatory measures.
Methods
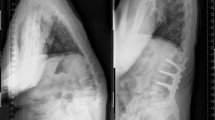
Adult spinal deformity (ASD) patients who were treated operatively, with a normal SVA (< ± 50 mm) at 6-week follow-up were included, who were then followed-up after 2 years. These only included patients with fusion of > 4 vertebrae extending to L5 or below. Six-week subgroups were made regarding pelvis orientation, relative pelvic version (RPV: anteversion, aligned, moderate or severe retroversion) with analysis of patient-related outcome measures (PROMs), complications and spino-pelvic sagittal parameters.
Results
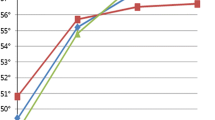
At 6 weeks, 140 patients met the inclusion criteria, 5 (3.6%) patients had anteversion, 59 (42.1%) were aligned, 60 (42.9%) had moderate retroversion and 16 (11.4%) patients had severe retroversion. Follow-up after 2 years demonstrated increased RPV in all groups except the severe RPV group who were more likely to develop SVA > 50 mm. Complications occurred in all groups. Significant 2-year differences were observed between moderate and severe RPV for back pain and PROMs but not between other RPV groups.
Conclusion
Adult spinal deformity patients with a normal SVA after spino-pelvic instrumentation carry a significant risk of retroversion progression post-operatively, followed by increased positive sagittal balance. Relative pelvic version (RPV) measurements when categorised into anteversion, aligned, moderate retroversion and severe retroversion at 6 weeks were predictive of PROMs at 2 years.




Similar content being viewed by others
References
Glassman SD, Berven S, Bridwell K et al (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine 30:682–688
Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, DeWald C, Mehdian H, Shaffrey C, Tribus C, Lafage V (2012) Scoliosis Research Society—Schwab adult spinal deformity classification: a validation study. Spine 37(12):1077–1082
Takemoto M, Boissière L, Vital JM, Pellisé F, Perez-Grueso FJ, Kleinstück F, Acaroglu ER, Alanay A, Obeid I (2017) Are sagittal spinopelvic radiographic parameters significantly associated with quality of life of adult spinal deformity patients? Multivariate linear regression analyses for pre-operative and short-term post-operative health-related quality of life. Eur Spine J 26(8):2176–2186
Takemoto M, Boissière L, Novoa F, Vital JM, Pellisé F, Pérez-Grueso FJ, Kleinstück F, Acaroglu ER, Alanay A, Obeid I, European Spine Study Group (2016) Sagittal malalignment has a significant association with postoperative leg pain in adult spinal deformity patients. Eur Spine J 25(8):2442–2451
Soroceanu A, Diebo BG, Burton D, Smith JS, Deviren V, Shaffrey C, Kim HJ, Mundis G, Ames C, Errico T, Bess S (2015) Radiographical and implant-related complications in adult spinal deformity surgery. Spine 40(18):1414–1421
Yilgor C, Sogunmez N, Yavuz Y, Abul K, Boissiére L, Haddad S, Obeid I, Kleinstück F, Pérez-Grueso FJ, Acaroğlu E, Mannion AF (2017) Relative lumbar lordosis and lordosis distribution index: individualized pelvic incidence–based proportional parameters that quantify lumbar lordosis more precisely than the concept of pelvic incidence minus lumbar lordosis. Neurosurg Focus 43(6):E5
Lafage V, Schwab F, Patel A et al (2009) Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine 34:E599-606
Preece SJ, Willan P, Nester CJ, Graham-Smith P, Herrington L, Bowker P (2008) Variation in pelvic morphology may prevent the identification of anterior pelvic tilt. J Manual Manip Ther 16(2):113–117
Yamato Y, Hasegawa T, Kobayashi S, Yasuda T, Togawa D, Arima H, Oe S, Iida T, Matsumura A, Hosogane N, Matsumoto M (2016) Calculation of the target lumbar lordosis angle for restoring an optimal pelvic tilt in elderly patients with adult spinal deformity. Spine 41(4):E211–E217
Fujishiro T, Boissière L, Cawley DT, Larrieu D, Gille O, Vital JM, Pellisé F, Pérez-Grueso FJ, Kleinstück F, Acaroglu E, Alanay A. Decision-making factors in the treatment of adult spinal deformity. European Spine Journal. 2018 Sep;27(9):2312–21.
Fujishiro T, Boissière L, Cawley DT, Larrieu D, Gille O, Vital JM, Pellisé F, Pérez-Grueso FJS, Kleinstück F, Acaroglu E, Alanay A, Obeid I, European Spine Study Group, ESSG (2019) Adult spinal deformity surgical decision-making score. Part 2: development and validation of a scoring system to guide the selection of treatment modalities for patients above 40 years with adult spinal deformity. Eur Spine J. https://doi.org/10.1007/s00586-019-06068-0
Maruo K, Ha Y, Inoue S, Samuel S, Okada E, Hu SS, Deviren V, Burch S, William S, Ames CP, Mummaneni PV (2013) Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine 38(23):E1469–E1476
Helgeson MD, Shah SA, Newton PO, Clements DH III, Betz RR, Marks MC, Bastrom T, Harms Study Group (2010) Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine 35(2):177–181
Yagi M, Rahm M, Gaines R, Maziad A, Ross T, Kim HJ, Kebaish K, Boachie-Adjei O, Complex Spine Study Group (2014) Characterization and surgical outcomes of proximal junctional failure in surgically treated patients with adult spinal deformity. Spine 39(10):E607–E614
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 30:346–353
Zhu Z, Xu L, Zhu F, Jiang L, Wang Z, Liu Z et al (2014) Sagittal alignment of spine and pelvis in asymptomatic adults: norms in Chinese populations. Spine 39:E1-6
Cawley DT, Larrieu D, Fujishiro T, Kieser D, Boissiere L, Acaroglu E, Alanay A, Kleinstück F, Pellisé F, Pérez-Grueso FS, Vital JM (2018) NRS20: combined back and leg pain score: a simple and effective assessment of adult spinal deformity. Spine 43(17):1184–1192
Alzakri A, Boissière L, Cawley DT, Bourghli A, Pointillart V, Gille O, Vital JM, Obeid I (2018) L5 pedicle subtraction osteotomy: indication, surgical technique and specificities. Eur Spine J 27(3):644–651
Ahern DP, Welch-Phillips A, Cawley DT, Butler JS (2020) Is multilevel anterior lumbar interbody fusion (ALIF) superior to pedicle subtraction osteotomy (PSO) for degenerative lumbar deformity? Clin Spine Surg 33(1):1–4
Sebaaly A, Sylvestre C, El Quehtani Y, Riouallon G, Larrieu D, Boussiere L, Steib JP, Roussouly P, Wolff S, Obeid I (2018) Incidence and risk factors for proximal junctional kyphosis. Clin Spine Surg 31(3):E178–E183
Le Huec JC, Leijssen P, Duarte M, Aunoble S (2011) Thoracolumbar imbalance analysis for osteotomy planification using a new method: FBI technique. Eur Spine J 20(5):669
Yilgor C, Sogunmez N, Yavuz Y, Boissiere L, Obeid I, Acaroglu E, Mannion AF, Pellise F, Alanay A (2017) Global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. Spine J 17(10):S155–S156
Funding
Depuy-Synthes funds were received by European Spine Study Group in support of this work. Relevant financial activities outside the submitted work: consultancy, royalties, grants. Funding was provided by Spineart, K2M, Medtronic, Zimmer Biomet, Alphatec Spine, Clariance.
Author information
Authors and Affiliations
Consortia
Contributions
DTC: material preparation, analysis, methodology, commented on previous versions of the manuscript, approved current version of manuscript. LB: material preparation, analysis, methodology, commented on previous versions of the manuscript, approved current version of manuscript. CY: material preparation, analysis, methodology, commented on previous versions of the manuscript, approved current version of manuscript. DL: material preparation, analysis, methodology, commented on previous versions of the manuscript, approved current version of manuscript. TF: material preparation, analysis, methodology, commented on previous versions of the manuscript, approved current version of manuscript. DK: material preparation, analysis, methodology, commented on previous versions of the manuscript, approved current version of manuscript. AA: study conception and design, data collection, methodology, funding acquisition, commented on previous versions of the manuscript, approved current version of manuscript. FK: study conception and design, data collection, methodology, funding acquisition, commented on previous versions of the manuscript, approved current version of manuscript. FSP: study conception and design, data collection, methodology, funding acquisition, commented on previous versions of the manuscript, approved current version of manuscript. FP: study conception and design, data collection, methodology, funding acquisition, commented on previous versions of the manuscript, approved current version of manuscript. IO: study conception and design, data collection, methodology, funding acquisition, commented on previous versions of the manuscript, approved current version of manuscript, supervision.
Corresponding author
Ethics declarations
Ethical approval
Institutional review board approval was obtained at each site for patient enrolment and data collection.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cawley, D.T., Boissiere, L., Yilgor, C. et al. Relative pelvic version displays persistent compensatory measures with normalised sagittal vertical axis after deformity correction. Spine Deform 9, 1449–1456 (2021). https://doi.org/10.1007/s43390-021-00345-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00345-z