Abstract
Purpose
Anterior vertebral body tethering (VBT) is a non-fusion surgical treatment for Adolescent Idiopathic Scoliosis requiring chest tube(s) (CT). We sought to assess the efficacy of post-op intravenous tranexamic acid (IV TXA) in reducing CT drainage and retention.
Methods
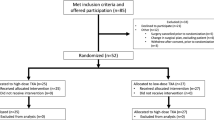
35 VBT patients received 24 h of post-op IV TXA (2 mg/kg/h) were compared to 49 who did not. Group comparisons were performed using Wilcoxon rank-sum and chi-squared tests. Multivariate linear regression analysis was used to assess the relationships between TXA and both CT drainage and retention time.
Results
There were no group differences at baseline (Table). CTs placed for thoracic (T) and thoracolumbar (TL) curves were assessed separately. For TH CT, there was less total CT drainage in the TXA group (TXA 569.4 ± 337.4 mL vs. Non-TXA 782.5 ± 338.9 mL; p = 0.003) and shorter CT retention time (TXA 3.0 ± 1.3 vs. Non-TXA 3.9 ± 1.4 days; p = 0.003). For TL CT, there was less total CT drainage in the TXA group (TXA 206.8 ± 152.2 mL vs. Non-TXA 395.7 ± 196.1 mL; p = 0.003) and shorter CT retention time (TXA 1.7 ± 1.3 vs. Non-TXA 2.7 ± 1.0 days; p = 0.001). Following multivariate analysis, use of TXA was the only significant predictor of both drainage in T and TL CTs (p = 0.012 and p = 0.002, respectively) as well as T and TL CT retention time (p = 0.008 and p = 0.009, respectively). There were no differences in LOS (p = 0.863) or ICU stay (p = 0.290).
Conclusion
IV TXA results in a significant decrease in CT drainage and retention time. CT retention is decreased by 1 day for those that receive TXA.
Level of evidence
III.
Similar content being viewed by others
Availability of data and material
Data will be maintained for this study for up to 7 years post publication as required by our institution’s review board.
Code availability
Not applicable.
References
Hoernschemeyer DG, Boeyer ME, Robertson ME et al (2020) Anterior vertebral body tethering for adolescent scoliosis with growth remaining: a retrospective review of 2 to 5- year postoperative results. J Bone Jt Surg 102(13):1169–1176. https://doi.org/10.2106/jbjs.19.00980
Newton PO, Bartley CE, Bastrom TP et al (2020) Anterior spinal growth modulation in skeletally immature patients with idiopathic scoliosis: a comparison with posterior spinal fusion at 2 to 5 years postoperatively. J Bone Jt Surg 102(9):769–777. https://doi.org/10.2106/jbjs.19.01176
Miyanji F, Pawelek J, Nasto LA et al (2020) Safety and efficacy of anterior vertebral body tethering in the treatment of idiopathic scoliosis. Bone Jt J 102-B(12):1703–1708. https://doi.org/10.1302/0301-620X.102B12.BJJ-2020-0426.R1
Samdani AF, Ames RJ, Kimball JS et al (2014) Anterior vertebral body tethering for idiopathic scoliosis: two-year results. Spine (Phila Pa 1976) 39(20):1688–1693. https://doi.org/10.1097/BRS.0000000000000472
Göttgens KWA, Siebenga J, Belgers EHJ et al (2011) Early removal of the chest tube after complete video-assisted thoracoscopic lobectomies. Eur J Cardio-thorac Surg 39(4):575–578. https://doi.org/10.1016/j.ejcts.2010.08.002
Wang D, Wang H-Y, Luo Z-Y et al (2019) Finding the optimal regimen for oral tranexamic acid administration in primary total hip arthroplasty. J Bone Jt Surg 101(5):438–445
Zhu X, Shi Q, Li D et al (2020) Two doses of tranexamic acid reduce blood loss in primary posterior lumbar fusion surgery: a randomized-controlled trial. Clin Spine Surg 33(10):E593–E597. https://doi.org/10.1097/BSD.0000000000000999
Neilipovitz DT (2004) Tranexamic acid for major spinal surgery. Eur Spine J 13:S62-65. https://doi.org/10.1007/s00586-004-0716-2
Slattery C, Kark J, Wagner T et al (2019) The use of tranexamic acid to reduce surgical blood loss: a review basic science, subspecialty studies, and the evolution of use in spine deformity surgery. Clin Spine Surg 32(2):46–50. https://doi.org/10.1097/BSD.0000000000000808
Goobie SM, Zurakowski D, Glotzbecker MP et al (2018) Tranexamic acid is efficacious at decreasing the rate of blood loss in adolescent scoliosis surgery: a randomized placebo-controlled trial. J Bone Jt Surg 100(23):2024–2032. https://doi.org/10.2106/JBJS.18.00314
Yuan Q, Zhi Z, Xu B (2016) Efficacy and safety of tranexamic acid in reducing blood loss in scoliosis surgery : a systematic review and meta-analysis. Eur Spine J 26:131–139. https://doi.org/10.1007/s00586-016-4899-0
Verma K, Errico T, Diefenbach C et al (2014) The relative efficacy of antifibrinolytics in adolescent idiopathic scoliosis. J Bone Jt Surg 96(10):e80
Peters A, Verma K, Slobodyanyuk K et al (2015) Antifibrinolytics reduce blood loss in adult spinal deformity surgery: a prospective, randomized controlled trial. Spine (Phila Pa 1976) 40(8):E443–E449. https://doi.org/10.1097/BRS.0000000000000799
Zhang Z, Wang L, Yang X et al (2021) The effect of multiple-dose oral versus intravenous tranexamic acid in reducing postoperative blood loss and transfusion rate after adolescent scoliosis surgery : a randomized controlled trial. Spine J 21(2):312–320. https://doi.org/10.1016/j.spinee.2020.10.011
Zhong J, Cao K, Wang B et al (2019) The perioperative efficacy and safety of tranexamic acid in adolescent idiopathic scoliosis. World Neurosurg 129:e726–e732. https://doi.org/10.1016/j.wneu.2019.05.261
Jones KE, Butler EK, Barrack T et al (2017) Tranexamic acid reduced the percent of total blood volume lost during adolescent idiopathic scoliosis surgery. Int J Spine Surg 11(4):212–217. https://doi.org/10.14444/4027
Pehlivanoglu T, Oltulu I, Ofluoglu E et al (2020) Thoracoscopic vertebral body tethering for adolescent idiopathic scoliosis: a minimum of 2 years’ results of 21 patients. J Pediatr Orthop 40(10):575–580. https://doi.org/10.1097/BPO.0000000000001590
Rushton PRP, Grevitt MP, Sell PJ (2015) Anterior or posterior surgery for right thoracic adolescent idiopathic scoliosis (AIS)? A prospective cohorts’ comparison using radiologic and functional outcomes. J Spinal Disord Tech 28(3):80–88. https://doi.org/10.1097/BSD.0b013e3182693e33
Mahaffey R, Wang L, Hamilton A et al (2013) A retrospective analysis of blood loss with combined topical and intravenous tranexamic acid after coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth 27(1):18–22. https://doi.org/10.1053/j.jvca.2012.08.004
Shrestha IK, Ruan TY, Lin L et al (2021) The efficacy and safety of high-dose tranexamic acid in adolescent idiopathic scoliosis: a meta-analysis. J Orthop Surg Res 16(1):1–9. https://doi.org/10.1186/s13018-020-02158-8
Martin K, Breuer T, Gertler R et al (2011) Tranexamic acid versus ε-aminocaproic acid: Efficacy and safety in paediatric cardiac surgery. Eur J Cardio-thoracic Surg 39(6):892–897. https://doi.org/10.1016/j.ejcts.2010.09.041
Zhou ZF, Zhang FJ, Huo YF et al (2017) Intraoperative tranexamic acid is associated with postoperative stroke in patients undergoing cardiac surgery. PLoS ONE 12(5):1–15. https://doi.org/10.1371/journal.pone.0177011
Johnson DJ, Johnson CC, Goobie SM et al (2017) High-dose versus low-dose tranexamic acid to reduce transfusion requirements in pediatric scoliosis surgery. J Pediatr Orthop 37(8):e552–e557. https://doi.org/10.1097/BPO.0000000000000820
Grant JA, Howard J, Luntley J et al (2009) Perioperative blood transfusion requirements in pediatric scoliosis surgery: the efficacy of tranexamic acid. J Pediatr Ortho 29(3):300–304. https://doi.org/10.1097/BPO.0b013e31819a85de
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
LE, SRS, LNH, JG, SG, JM, SD, BL: Made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data. Drafted the work or revised it critically for important intellectual content. Approved the version to be published. Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Lonner reports personal fees and royalty fees from Zimmer Biomet for The Tether implant. Dr. Lonner also reports personal fees, non-financial support and other from Depuy Synthes, personal fees, equity, and non-financial support from OrthoPediatrics, stocks/stock options from Spine Search, grants and other from Setting Scoliosis Straight Foundation, outside the submitted work. Dr. Hodo reports non-financial leadership roles as Executive Council, Section on Hospital Medicine, American Academy of Pediatrics and Executive Council, Pediatric Special Interest Group, Society of Hospital Medicine, out the submitted work. The remaining authors have no disclosures to report.
Ethical approval
This work was approved by the Institutional Review Board at Mount Sinai Hospital.
Consent to participate
This work was performed under a waiver of informed consent approved by the Institutional Review Board at Mount Sinai Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Eaker, L., Selverian, S.R., Hodo, L.N. et al. Post-operative tranexamic acid decreases chest tube drainage following vertebral body tethering surgery for scoliosis correction. Spine Deform 10, 811–816 (2022). https://doi.org/10.1007/s43390-022-00492-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00492-x