Abstract
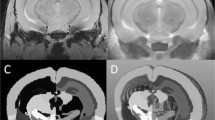
Experimental autoimmune encephalomyelitis (EAE) is utilized as an animal model for multiple sclerosis (MS). In both EAE and MS, activated T-lymphocytes specific for self-antigens present in myelin are linked to CNS inflammation and the breakdown of the blood-brain barrier (BBB) to peripheral blood leukocytes and plasma proteins, predominately in myelin rich white matter. One aspect of MS that has received relatively little attention is the finding that certain CNS regions are more likely than others to develop disease in different patient populations. Understanding the factors predisposing specific brain regions to autoimmune attack, or protecting other regions, would provide a better understanding of the disease as a process, and may also offer additional targets for therapeutic development. EAE offers a model to search for these factors and the first step in such a process is to identify the brain regions that are susceptible to EAE. Until recently the spinal cord in rodents has been considered the region most susceptible to EAE, with disease in more rostral regions occurring later and with reduced severity. However a more recent study has shown that the cerebellum of SJL/J mice, like the spinal cord, is especially susceptible to BBB breakdown in EAE. Although many factors known to be involved in BBB formation and breakdown remain to be assessed for their possible role in increasing the susceptibility of the cerebellum, one potentially important factor is the location of venules, which are the most affected vascular elements in inflamed tissue. There is a prevalence of large EAE susceptible venules traveling in the myelin rich white matter tracts in SJL/J mouse cerebellar cortex, indicating that the vascularization of this tissue may contribute to the increased susceptibility to inflammation in response to autoimmune attacks directed against CNS myelin.
Similar content being viewed by others
References
Tonra JR., Reiseter BS., Kolbeck R, et al. Comparison of the timing of acute blood-brain barrier breakdown to rabbit immunoglobin G in the cerebellum and spinal cord of mice with experimental autoimmune encephalomyelitis. J Comp Neurol 2001; 430: 131–144.
Oldendorf WH., Cornford ME., Brown WJ. The large apparent work capability of the blood-brain barrier: a study of the mitochondrial content of capillary endothelial cells in brain and other tissues of the rat. Ann Neurol 1976; 1: 409–417.
Van Deurs B, Ropke C, Westergaard E. Ultrastructure and permeability of lymph node microvasculature in the mouse. Cell Tiss Res 1976; 168: 507–525.
Stewart PA, Wiley MJ. Developing nervous tissue induces formation of blood-brain barrier characteristics in invading endothelial cells: a study using quail-chick transplantation chimeras. Dev Biol 1981; 84: 183–192.
Adinolfi M The permeability of the blood-CSF barrier during foetal life in man and rat and the effect of brain antibodies on the development of the CNS. In: Hemmings, W.A. editor. Protein transmission through living membranes. Amsterdam: Elsevier/North-Holland Biomedical Press, 1979: 349–364.
Stewart PA, Hayakawa EM. Interendothelial junctional changes underlie the developmental ‘tightening’ of the blood-brain barrier. Dev Brain Res 1987; 32: 271–281.
Robertson PL, DuBois M, Bowman PD, Goldstein GW. Angiogenesis in developing rat brain: an in vivo and in vitro study. Dev Brain Res 1985; 23: 219–223.
Tonra JR, Mendell LM. Rabbit IgG distribution in skin, spinal cord and DRG following systemic injection in rat. J Neuroimmunol 1997; 80: 97–105.
Cassella JP, Lawrenson JG, Allt G, Firth JA. Ontogeny of four blood-brain barrier markers: an immunocytochemical comparison of pial and cerebral cortical microvessels. J Anat 1996; 189: 407–415.
Ghabriel MN, Zhu C, Hermanis G, Allt G. Immunological targeting of the endothelial barrier antigen (EBA) in vivo leads to opening of the blood-brain barrier. Brain Res 2000; 878: 127–135.
Bar T, Wolff JR. Morphometry of interendothelial and glio-vascular contacts of rat brain capillaries during postnatal development. In: Lewis DH editor. Recent advances in basic microcirculatory research. Basel: S. Karger, 1976: 514–517.
Janzer RC, Raff MC. Astrocytes induce blood-brain barrier properties in endothelial cells. Nature 1987; 325: 253–257.
Holash JA, Noden DM, Stewart PA. Re-evaluating the role of astrocytes in blood-brain barrier induction. Dev Dyn 1993; 197: 14–25.
Rubin LL, Hall DE, Porter S et al. A cell culture model of the blood-brain barrier. J Cell Biol 1991; 115: 1725–1735.
Harik SI, Sharma VK, Wetherbee JR et al. Adrenergic and cholinergic receptors of cerebral microvessels. J Cereb Blood Flow Metab 1981; 1: 329–338.
Rubin LL, Staddon JM. The cell biology of the blood-brain barrier. Ann Rev Neurosci 1999; 22: 11–28.
Hirase T, Staddon JM, Saitou M et al. Occludin as a possible determinant of tight junction permeability in endothelial cells. J Cell Sci 1997; 110: 1603–1613.
Reese TS, Karnovsky MJ. Fine structural localization of a blood-brain barrier to exogenous peroxidase. J Cell Biol 1967; 34: 207–217.
Gross PM. Circumventricular organ capillaries. Prog Brain Res 1992; 91: 219–233.
Banks WA. Physiology and pathology of the blood-brain barrier: implications for microbial pathogenesis, drug delivery and neurodegenerative disorders. J Neurovirology 1999; 5: 538–555.
Drewes LR. What is the blood-brain barrier? A molecular perspective. In Roach RC editor. Hypoxia: Into the next millennium. New York: Kluwer Academic/Plenum Publishing, 1999: 111–122.
Knopf PM, Cserr HF., Nolan SC., Wu TY., Harling-Berg CJ. Physiology and immunology of lymphatic drainage of interstitial and cerebrospinal fluid from the brain. Neuropathol Appl Neurobiol 1995; 21: 175–180.
Knopf PM, Harling-Berg CJ., Cserr HF, et al. Antigen-dependent intrathecal antibody synthesis in the normal rat brain: tissue entry and local retention of antigen-specific B cells. J Immunol 1998; 161: 692–701.
Hickey WF, Hsu BL., Kimura H. T-lymphocyte entry into the central nervous system. J Neurosci Res 1991; 28: 254–260.
Dopp JM, Breneman SM, Olschowka JA. Expression of ICAM-1, VCAM-1, L-selectin, and leukosialin in the mouse central nervous system during the induction and remission stages of experimental allergic encephalomyelitis. J Neuroimmunol 1994; 54: 129–144.
Raine CS, Cannella B, Duijvestijn AM, Cross AH. Homing to central nervous system vasculature by antigen-specific lymphocytes II. Lymphocyte/endothelial cell adhesion during the initial stages of autoimmune demyelination. Lab Invest 1990; 63: 476–489.
Namer IJ, Steibel J, Poulet P, et al. Blood-brain barrier breakdown in MBP-specific T cell induced experimental allergic encephalomyelitis. A quantitative in vivo MRI study. Brain 1993; 116: 147–159.
Andersson PB, Perry VH, Gordon S. The acute inflammatory response to lipopolysaccharide in CNS parenchyma differs from that in other body tissues. Neurosci 1992; 48: 169–186.
Miller DW. Immunobiology of the blood-brain barrier. J Neu- rovirology 1999; 5: 570–57.
Hellings N, Baree M, Verhoeven C, et al. T-cell reactivity to multiple myelin antigens in multiple sclerosis patients and healthy controls. J Neurosci Res 2001; 63: 290–302.
Bajramovic JJ, Plomp AC, van der Goes A, et al. Presentation of αβ-crystallin to T cells in active multiple sclerosis lesions: an early event following inflammatory demyelination. J Immunol 2000; 164: 4359–4366.
Poser CM. Multiple sclerosis observations and reflections—a personal memoir. J Neurol Sci 1992; 107: 127–140.
Cross AH, O’Mara T, Raine CS. Chronologic localization of myelin-reactive cells in the lesions of relapsing EAE: implications for the study of multiple sclerosis. Neurology 1993; 43: 1028–1033.
Brocke S, Gijbels K, Steinman L. Experimental autoimmune encephalomyelitis in the mouse. In: Cohen IR editor. Autoimmune disease models: a guidebook. San Diego, CA: Academic Press, Inc., 1994: 1–14.
Cutler RWP, Lorenzo AV, Barlow CF. Brain vascular permeability to I125 gamma globulin and leukocytes in allergic encephalomyelitis. J Neuropathol Exp Neurol 1967; 26: 558–571.
Linthicum DS, Mackay IR, Carnegie PR. Measurement of cell- mediated inflammation in experimental murine autoimmune encephalomyelitis by radioisotopic labeling. J Immunol 1979; 123: 1799–1805.
Brown A, McFarlin DE, Raine CS. Chronologic neuropathology of relapsing experimental allergic encephalomyelitis in the mouse. Lab Invest 1982; 46: 171–185.
Gijbels K, Brocke S, Abrams JS, Steinman L. Administration of neutralizing antibodies to interleukin-6 (IL-6) reduces experimental autoimmune encephalomyelitis and is associated with elevated levels of IL-6 bioactivity in central nervous system and circulation. Mol Med 1995; 1: 795–805.
Stinissen P, Raus J, Zhang J. Autoimmune pathogenesis of multiple sclerosis: role of autoreactive T lymphocytes and new immunotherapeutic strategies. Crit Rev Immunol 1997; 17: 33–75.
Hickey WF. The pathology of multiple sclerosis: a historical perspective. J Neuroimmunol 1999; 98: 37–44.
Stone LA, Albert PS, Smith ME, et al. Changes in the amount of diseased white matter over time in patients with relapsing-remitting multiple sclerosis. Neurology 1995; 45: 1808–1814.
Evangelou N, Konz D, Esiri MM, Smith S, Palace J, Matthews PM. Regional axonal loss in the corpus callosum correlates with cerebral white matter lesion volume and distribution in multiple sclerosis. Brain 2000; 123: 1845–1849.
Tan IL, van Schijndel RA, Pouwels PJW, et al. MR venography of multiple sclerosis. Am J Neuroradiol 2000; 21: 1039–1042.
Renno T, Krakowski M, Piccirillo C, Lin J-y, Owens T. TNF-α expression by resident microglia and infiltrating leukocytes in the central nervous system of mice with experimental allergic encephalomyelitis: regulation by Th1 cytokines. J Immunol 1995; 154: 944–953.
Jensen MA, Dayal A, Arnason GW. Cytokine secretion by gd and ab T cells in monophasic experimental autoimmune encephalomyelitis. J Autoimmunity 1999; 12: 73–80.
Steinman L, Solomon D, Lim M, Zamvil S, Sriram S. Prevention of experimental allergic encephalitis with in vivo administration of anti I-A antibody: decreased accumulation of radiolabelled lymph node cells in the central nervous system. J Neuroimmunol 1983; 5: 91–97.
Greer JM, Sobel RA, Sette A, Southwood S, Lees MB, Kuchroo VK. Immunogenic and encephalitogenic epitope clusters of myelin proteolipid protein. J Immunol 1996; 156: 371–379.
Hickey WF, Kimura H. Perivascular microglial cells of the CNS are bone marrow-derived and present antigen in vivo. Science 1988; 239: 290–292.
Olerup O, Hillert J. HLA class II-associated genetic susceptibility in multiple sclerosis: a critical evaluation. Tissue Antigens 1991; 38: 1–15.
Kira J-I, Kanai T, Nishimura Y, et al. Western versus asian types of multiple sclerosis: immunogenetically and clinically distinct disorders. Ann Neurol 1996; 40: 569–574.
Happ MP, Wettstein P, Dietzschold B, Heber-Katz E. Genetic control of the development of experimental allergic encephalomyelitis in rats: separation of MHC and non-MHC gene effects. J Immunol 1988; 141: 1489–1494.
Angelov DN, Walther M, Streppel M, Guntinas-Lichius O, Neiss WF. The cerebral perivascular cells. Adv Anat Embryol Cell Biol 1998; 147: 1–87.
Sobel RA, Blanchette BW, Bhan AK, Colvin RB. The immunopathology of experimental allergic encephalomyelitis II. Endothelial cell Ia increases prior to inflammatory cell infiltration. J Immunol 1984; 132: 2402–2407.
Traugott U, Scheinberg LC, Raine CS. On the presence of Iapositive endothelial cells and astrocytes in multiple sclerosis lesions and its relevance to antigen presentation. J Neuroimmunol 1985; 8: 1–14.
Sobel RA, Natale JM, Schneeberger EE. The immunopathology of acute experimental allergic encephalomyelitis. IV. An ultrastructural immunocytochemical study of class II major histocompatibility complex molecule (Ia) expression. J Neuropathol Exp Neurol 1987; 46: 239–249.
Butter C, Healy DG, Agha N, Turk JL. An immunoelectron microscopical study of the expression of Class II MHC and a T lymphocyte surface marker during chronic relapsing experimental allergic encephalomyelitis. J Neuroimmunol 1988; 20: 45–51.
Ong WY, Leong SK, Garey LJ, Tan KK, Zhang HF. A light and electron microscopic study of HLA-DR positive cells in the human cerebral cortex and subcortical white matter. J Brain Res 1995; 36: 553–563.
Wong GHW, Bartlett PF, Clark-Lewis I, Battye F, Schrader JW. Inducible expression of H-2 and Ia antigens on brain cells. Nature 1984; 310: 688–691.
Vass K, Lassmann H, Wisniewski HM, Iqbal K. Ultracytochemical distribution of myelin basic protein after injection into the cerebrospinal fluid: evidence for transport through the blood-brain barrier and binding to the luminal surface of cerebral veins. J Neurol Sci 1984; 63: 423–433.
McCombe PA, de Jersey J, Pender MP. Inflammatory cells, microglia and MHC class II antigen-positive cells in the spinal cord of lewis rats with acute and chronic relapsing experimental autoimmune encephalomyelitis. J Neuroimmunol 1994; 51: 153–167.
Bauer J, Huitinga I, Zhao W, Lassmann H, Hickey WF, Dijkstra CD. The role of macrophages, perivascular cells, and microglial cells in the pathogenesis of experimental autoimmune encephalomyelitis. Glia 1995; 15: 437–446.
Panek RB, Benveniste EN. Class II MHC gene expression in microglia: regulation by the cytokines IFN-γ, TNF-a, and TGF- β. J Immunol 1995; 154: 2846–2854.
Lampert P, Carpenter S. Electron microscopic studies on the vascular permeability and the mechanism of demyelination in experimental allergic encephalomyelitis. J Neuropath Exp Neurol 1965; 24: 11–24.
Pober JS, Gimbrone MA Jr., Lapierre LA, et al. Overlapping patterns of activation of human endothelial cells by interleukin 1, tumor necrosis factor, and immune interferon. J Immunol 1986; 137: 1893–1896.
Wong D, Prameya R, Dorovini-Zis K. In vitro adhesion and migration of T lymphocytes across monolayers of human brain microvessel endothelial cells: regulation by ICAM-1, VCAM-1, E-selectin and PECAM-1. J Neuropathol Exp Neurol 1999; 58: 138–152.
Kawai K, Kobayashi Y, Shiratori M, et al. Intrathecal administration of antibodies against LFA-1 and against ICAM-1 suppresses experimental allergic encephalomyelitis in rats. Cell Immunol 1996; 171: 262–268.
Meeson AP, Piddlesden S, Morgan BP, Reynolds R. The distribution of inflammatory demyelinated lesions in the central nervous system of rats with antibody-augmented demyelinating experimental allergic encephalomyelitis. Exp Neurol 1994; 129: 299–310.
Muller DM, Pender MP, Greer JM. A neuropathological analysis of experimental autoimmune encephalomyelitis with predominant brain stem and cerebellar involvement and differences between active and passive induction. Acta Neuropathol 2000; 100: 174–182.
Zaman MS, Hupp EW, Lancaster FE. Brain myelination in rats treated with ionizing radiation in utero. J Environ Sci Health 1992; B27: 621–638.
Williams KA, Deber CM. The structure and function of central nervous system myelin. Crit Rev Clin Lab Sci 1993; 30: 29–64.
Sampugna J, Clements J, Carter TP, Campagnoni AT. Comparison of lipids in total brain tissue from five mouse genotypes. J Neurobiol 1975; 6: 259–266.
Hirano A, Dembitzer HM, Becker NH, Levine S, Zimmerman HM. Fine structural alterations of the blood-brain barrier in experimental allergic encephalomyelitis. J Neuropath Exp Neurol 1970; 29: 432–440.
Jung U, Norman KE, Scharffetter-Kochanek K, Beaudet AL, Ley K. Transit time of leukocytes rolling through venules controls cytokine-induced inflammatory cell recruitment in vivo. J Clin Invest 1998; 102: 1526–1533.
Kunkel EJ, Dunne JL, Ley K. Leukocyte arrest during cytokine- dependent inflammation in vivo. J Immunol 2000; 164: 3301–3308.
Cunningham ET, Wada E, Carter DB, Tracey DE, Battey JF, De Souza EB. In situ histochemical localization of type I inter-leukin-1 receptor messenger RNA in the central nervous system, pituitary, and adrenal gland of the mouse. J Neurosci 1992; 12: 1101–1114.
Yi ES, Ulich TR. Endotoxin, interleukin-1, and tumor necrosis factor cause neutrophil-dependent microvascular leakage in postcapillary venules. Am J Pathol 1992; 140: 659–663.
Duijvestijn AM, Kerkhove M, Bargatze RF, Butcher EC. Lymphoid tissue- and inflammation-specific endothelial cell differentiation defined by monoclonal antibodies. J Immunol 1987; 138: 713–719.
Cannella B, Cross AH, Raine CS. Relapsing autoimmune demyelination: a role for vascular addressins. J Neuroimmunol 1991; 35: 295–300.
Butter C, Baker D, O’Neill JK, Turk JL. Mononuclear cell trafficking and plasma protein extravasation into the CNS during chronic relapsing experimental allergic encephalomyelitis in Biozzi AB/H mice. J Neurol Sci 1991; 104: 9–12.
Smith ME, Stone LA, Albert PS, et al. Clinical worsening in multiple sclerosis is associated with increased frequency and area of gadopentetate dimeglumine-enhancing magnetic resonance imaging lesions. Ann Neurol 1993; 33: 480–489.
Hawkins CP, Munro PMG, MacKenzie F, et al. Duration and selectivity of blood-brain barrier breakdown in chronic relapsing experimental allergic encephalomyelitis studied by gadolinium- DTPA and protein markers. Brain 1990; 113: 365–378.
Adams CWM. The onset and progression of the lesion in multiple sclerosis. J Neurol Sci 1975; 25: 165–182.
Duijvestijn AM, Schreiber AB, Butcher EC. Interferon-γ regulates an antigen specific for endothelial cells involved in lymphocyte traffic. Proc Natl Acad Sci USA 1986; 83: 9114–9118.
Oshima T, Laroux FS, Coe LL, et al. Interferon-γ and interleukin-10 reciprocally regulate endothelial junction integrity and barrier function. Microvasc Res 2001; 61: 130–143.
Bansil S, Singhal BS, Ahuja GK, et al. Comparison between multiple sclerosis in India and the United States: a case-control study. Neurol 1996; 46: 385–387.
Kira J-i, Yamasaki K, Horiuchi I, Ohyagi Y, Taniwaki T, Kawano Y. Changes in the clinical phenotypes of multiple sclerosis during the past 50 years in Japan. J Neurol Sci 1999; 166: 53–57.
Oldendorf WH, Towner HF. Blood-brain barrier and DNA changes during the evolution of experimental allergic encephalomyelitis. J Neuropathol Exp Neurol 1974; 33: 616–631.
De Rosbo NK, Bernard CCA, Simmons RD, Carnegie PR. Concomitant detection of changes in myelin basic protein and permeability of blood-spinal cord barrier in acute experimental autoimmune encephalomyelitis by electroimmunoblotting. J Neuroimmunol 1985; 9: 349–361.
Leibowitz S, Kennedy L. Cerebral vascular permeability and cellular infiltration in experimental allergic encephalomyelitis. Immunol 1972; 22: 859–869.
Kristensson K, Wisniewski HM. Chronic relapsing experimental allergic encephalomyelitis: studies in vascular permeability changes. Acta Neuropath (Berlin) 1977; 39: 189–194.
Ormerod IEC, Miller DH, McDonald WI, et al. The role of NMR imaging in the assessment of multiple sclerosis and isolated neurological lesions: a quantitative study. Brain 1987; 110: 1579–1616.
Lange W, Halata Z. Comparative studies on the pre-and post- terminal blood vessels in the cerebellar cortex of rhesus monkey, cat, and rat. Anat Embryol 1979; 158: 51–62.
Conradi NG, Engvall J, Wolff JR. Angioarchitectonics of rat cerebellar cortex during pre- and postnatal development. Acta Neuropathol (Berlin) 1980; 50: 131–138.
Duvernoy HM, Delon S, Vannson JL. Cortical blood vessels of the human brain. Brain Res Bull 1981; 7: 519–579.
Roggendorf W, Cervos-Navarro J. Characterization of venules in the brain. Adv Neurol 1978; 20: 39–46.
Kidd D, Barkhof F, McConnell R, Algra PR, Allen IV, Revesz T. Cortical lesions in multiple sclerosis. Brain 1999; 122: 17–26.
Cassella JP, Lawrenson JG, Lawrence L, Firth JA. Differential distribution of an endothelial barrier antigen between the pial and cortical microvessels of the rat. Brain Res 1997; 744: 335–338.
Sternberger NH, Sternberger LA, Kies MW, Shear CR. Cell surface endothelial proteins altered in experimental allergic encephalomyelitis. J Neuroimmunol 1989; 21: 241–248.
Sobel RA, Greer JM, Kuchroo VK. Autoimmune responses to myelin proteolipid protein. Neurochem Res 1994; 19: 915–921.
Tveten L. Spinal cord vascularity V. The venous drainage of the spinal cord of the rat. Acta Radiol Diag 1976; 17: 653–662.
Bar T. The vascular system of the cerebral cortex. Adv Anat Embryol Cell Biol 1980; 59: I-VI, 1–62.
Ambach G, Toldi J, Feher O, Joo F, Wolff JR. Spatial correlation between sensory regions and the drainage fields of pial veins in rat cerebral cortex. Exp Brain Res 1986; 61: 540–548.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tonra, J.R. Cerebellar susceptibility to experimental autoimmune encephalomyelitis in SJL/J mice: Potential interaction of immunology with vascular anatomy. Cerebellum 1, 57–68 (2002). https://doi.org/10.1080/147342202753203096
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1080/147342202753203096