Abstract
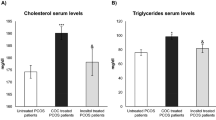
To determine whether metformin, when given to women with polycystic ovary syndrome (PCOS), promotes folliculogenesis by prompting a drop in free sex steroids resulting in a compensatory follicle stimulating hormone (FSH) rise, we conducted a randomized, double-blind, placebo-controlled crossover clinical trial. Eight mid-reproductive age PCOS participants with mean obese body mass index (BMI) and normal glucose tolerance received 8 weeks of metformin, given in a step-up fashion to a maximum dose of 2000 mg daily or placebo with daily urine sampling, 4–6 weeks washout, and crossover to the remaining arm for 8 weeks. To confirm the effects of metformin on glucose and other metabolic markers, a hyperinsulinemic, euglycemic 3-dose clamp (physiologic: 30 mU/m2 per minute, high: 400 mU/m2 per minute) followed each treatment. Urinary FSH, luteinizing hormone (LH), or pregnanediol glucuronide (Pdg) did not differ by treatment. Glucose disposal, endogenous glucose production, BMI, ovulation rates, serum sex steroids, free fatty acids, and lipids did not significantly differ by treatment, despite good evidence for compliance with the protocol. During the clamp, high-dose insulin administration was associated with an acute drop in serum LH. We conclude that short-term, high-dose metformin exerts minimal effects on both metabolic markers and reproductive hormones in a small sample of overall morbidly obese women.
Similar content being viewed by others
References
Knochenhauer ES, Key TJ, Kahsar-Miller M, Waggoner W, Boots LR, Azziz R. Prevalence of the polycystic ovary syndrome in unselected black and white women of the southeastern united states: a prospective study. J Clin Endocrinol Metab. 1998;83(9):3078–3082.
Yildiz BO, Knochenhauer ES, Azziz R. Impact of obesity on the risk for polycystic ovary syndrome. J Clin Endocrinol Metab. 2008;93(1):162–168.
Azziz R, Woods KS, Reyna R, Key TJ, Knochenhauer ES, Yildiz BO. The prevalence and features of the polycystic ovary syndrome in an unselected population. J Clin Endocrinol Metab. 2004;89(6):2745–2749.
Dumesic DA, Abbott DH, Padmanabhan V. Polycystic ovary syndrome and its developmental origins. Rev Endocr Metab Disord. 2007;8(2):127–141.
Waldstreicher J, Santoro NF, Hall JE, Filicori M, Crowley WF Jr. Hyperfunction of the hypothalamicpituitary axis in women with polycystic ovarian disease: indirect evidence for partial gonadotroph desensitization. J Clin Endocrinol Metab. 1988;66(1):165–172.
Zumoff B, Freeman R, Coupey S, Saenger P, Markowitz M, Kream J. A chronobiologic abnormality in luteinizing hormone secretion in teenage girls with the polycystic-ovary syndrome. N Engl J Med. 1983;309(20):1206–1209.
Nestler JE, Jakubowicz DJ, de Vargas AF, Brik C, Quintero N, Medina F. Insulin stimulates testosterone biosynthesis by human thecal cells from women with polycystic ovary syndrome by activating its own receptor and using inositolglycan mediators as the signal transduction system. J Clin Endocrinol Metab. 1998;83(6):2001–2005.
Lord JM, Flight IH, Norman RJ. Insulin-sensitising drugs (metformin, troglitazone, rosiglitazone, pioglitazone, D-chiro-inositol) for polycystic ovary syndrome. Cochrane Database Syst Rev. 2003;(3):CD003053.
Nestler JE, Jakubowicz DJ, Evans WS, Pasquali R. Effects of metformin on spontaneous and clomiphene-induced ovulation in the polycystic ovary syndrome. N Engl J Med. 1998;338(26):1876–1880.
Nestler JE, Jakubowicz DJ. Decreases in ovarian cytochrome P450c17{alpha} activity and serum free testosterone after reduction of insulin secretion in polycystic ovary syndrome. N Engl J Med. 1996;335(9):617–623.
Nestler JE, Powers LP, Matt DW, et al. A direct effect of hyperinsulinemia on serum sex hormone-binding globulin levels in obese women with the polycystic ovary syndrome. J Clin Endocrinol Metab. 1991;72(1):83–89.
Shadid S, Kanaley J, Sheehan M, Jensen M. Basal and insulin-regulated free fatty acid and glucose metabolism in humans. Am J Physiol Endocrinol Metab. 2007;292(6):E1770–1774.
Al Majali K, Cooper MB, Staels B, Luc G, Taskinen MR, Betteridge DJ. The effect of sensitisation to insulin with pioglitazone on fasting and postprandial lipid metabolism, lipoprotein modification by lipases, and lipid transfer activities in type 2 diabetic patients. Diabetologia. 2006;49(3):527–537.
Zawadski JK, Dunaif A. Diagnostic criteria for polycystic ovary syndrome: towards a rational approach. In: Dunaif A, Givens JR, Haseltine FP, Merriam GR, eds. Polycystic Ovary Syndrome. Boston: Blackwell Scientific; 1992:377–384.
Hatch R, Rosenfield RL, Kim MH, Tredway D. Hirsutism: implications, etiology, and management. Am J Obstet Gynecol. 1981;140:815–830.
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15(7):539–553.
Diamond MP, Jacob R, Connolly-Diamond M, DeFronzo RA. Glucose metabolism during the menstrual cycle. Assessment with the euglycemic, hyperinsulinemic clamp. J Reprod Med. 1993;38(6):417–421.
Thornton KL, DeFronzo RA, Sherwin RS, Diamond MP. Micronized estradiol and progesterone: effects on carbohydrate metabolism in reproductive-age women. J Soc Gynecol Investig. 1995;2(4):643–652.
Saketos M, Sharma N, Adel T, Raghuwanshi M, Santoro N. Time-resolved immunofluorometric assay and specimen storage conditions for measuring urinary gonadotropins. Clin Chem. 1994;40(5):749–753.
Santoro N, Brown J, Adel T, Skurnick J. Characterization of reproductive hormonal dynamics in the perimenopause. Journal of Clinical Endocrinology & Metabolism. 1996;81(4): 1495–1501.
Steele R. Influences of glucose loading and of injected insulin on hepatic glucose output. Ann N Y Acad Sci. 1959;82: 420–430.
Bier DM, Arnold KJ, Sherman WR, Holland WH, Holmes WF, Kipnis DM. In-vivo measurement of glucose and alanine metabolism with stable isotopic tracers. Diabetes. 1977;26(11):1005–1015.
Brown JB. Pituitary control of ovarian function—concepts derived from gonadotrophin therapy. Aust N Z J Obstet Gynaecol. 1978;18(1):46–54.
Diamanti-Kandarakis E, Kouli C, Tsianateli T, Bergiele A. Therapeutic effects of metformin on insulin resistance and hyperandrogenism in polycystic ovary syndrome. Eur J Endocrinol. 1998;138(3):269–274.
Glueck CJ, Wang P, Fontaine R, Tracy T, Sieve-Smith L. Metformin-induced resumption of normal menses in 39 of 43 (91%) previously amenorrheic women with the polycystic ovary syndrome. Metabolism. 1999;48(4):511–519.
Nestler JE, Jakubowicz DJ. Lean women with polycystic ovary syndrome respond to insulin reduction with decreases in ovarian P450c17 alpha activity and serum androgens. J Clin Endocrinol Metab. 1997;82(12):4075–4079.
Lord J, Thomas R, Fox B, Acharya U, Wilkin T. The effect of metformin on fat distribution and the metabolic syndrome in women with polycystic ovary syndrome- a randomised, double-blind, placebo-controlled trial. BJOG: An International Journal of Obstetrics & Gynaecology. 2006;113(7):817–824.
Legro RS, Barnhart HX, Schlaff WD, et al. Clomiphene, metformin, or both for infertility in the polycystic ovary syndrome. N Engl J Med. 2007;356(6):551–566.
Ehrmann DA, Cavaghan MK, Imperial J, Sturis J, Rosenfield RL, Polonsky KS. Effects of metformin on insulin secretion, insulin action, and ovarian steroidogenesis in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 1997;82(2):524–530.
Acbay O, Gundogdu S. Can metformin reduce insulin resistance in polycystic ovary syndrome? Fertil Steril. 1996;65(5):946–949.
Palomba S, Falbo A, Orio Jr F, Tolino A, Zullo F. Efficacy predictors for metformin and clomiphene citrate treatment in anovulatory infertile patients with polycystic ovary syndrome. Fertility and Sterility. In Press.
Maciel GAR, Soares junior JM, Alves da Motta, et al. Nonobese women with polycystic ovary syndrome respond better than obese women to treatment with metformin. Fertil Steril. 2004;81(2):355–360. May 9, 2009. http://journals.ohiolink.edu/ejc/article.cgi?issn=00150282&issue=v81i0002&article=355_nwwposowttwm.
Moghetti P, Castello R, Negri C, et al. Metformin effects on clinical features, endocrine and metabolic profiles, and insulin sensitivity in polycystic ovary syndrome: a randomized, double-blind, placebo-controlled 6-month trial, followed by open, long-term clinical evaluation. J Clin Endocrinol Metab. 2000;85(1):139–146.
Srinivasan S, Ambler GR, Baur LA, et al. Randomized, controlled trial of metformin for obesity and insulin resistance in children and adolescents: improvement in body composition and fasting insulin. J Clin Endocrinol Metab. 2006;91(6): 2074–2080.
Morel Y, Golay A, Perneger T, et al. Metformin treatment leads to an increase in basal, but not insulin-stimulated, glucose disposal in obese patients with impaired glucose tolerance. Diabetic Med. 1999;16(8):650–655.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aubuchon, M., Lieman, H., Stein, D. et al. Metformin Does Not Improve the Reproductive or Metabolic Profile in Women With Polycystic Ovary Syndrome (PCOS). Reprod. Sci. 16, 938–946 (2009). https://doi.org/10.1177/1933719109340925
Published:
Issue Date:
DOI: https://doi.org/10.1177/1933719109340925