Abstract
Background
Tc-99-sestamibi scanning is utilized to determine whether patients with primary hyperparathyroidism (HPT) are candidates for minimally invasive parathyroidectomy (MIP). However, if the result of this scan is negative, many surgeons recommend bilateral parathyroid exploration because of possible multi-gland disease. The objectives of this study were to determine whether patients with primary HPT and negative sestamibi scans can benefit from additional imaging studies and are still potential candidates for MIP.
Methods
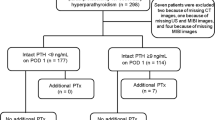
Between March 2001 and April 2006, 578 consecutive patients with HPT underwent parathyroidectomy by a single surgeon. Pre-operative sestamibi scans had been done in 458 (79%) of these patients, 90 (20%) of which had negative results. These patients formed our study cohort.
Results
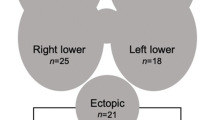
Of the 90 patients, 60 (67%) had a single adenoma, 17 (19%) double adenomas and 13 (14%) 3- to 4-gland hyperplasias. In 74 (82%) patients, localization was further investigated with one or more studies including thallium subtraction scans (n = 30), ultrasound (n = 15) and intra-operative internal jugular venous sampling (n = 49). Additionally, the use of radio-guided techniques intra-operatively facilitated minimally invasive techniques. Of these 90 patients, 47 had positive results from preoperative studies, including 12 positive thallium, 5 positive ultrasound and 13 positive internal jugular sampling results. In addition, positive results were observed for 17 patients using radio-probe techniques in the operating room. Accordingly, minimally invasive techniques were attempted in these 47 patients; 42 (89%) had single adenomas and in 5 the technique was converted to bilateral exploration for double adenoma/hyperplasia. In the setting of a negative sestamibi, the sensitivities of thallium scans and ultrasound were 30% and 27%, respectively. The overall cure rate in the 90 patients with negative sestamibi scans was 99%.
Conclusion
In patients with primary HPT and a negative sestamibi scan, most patients (67%) will have a single adenoma. These patients benefitted from additional localization tests, which yielded a positive result in 52% of patients. Therefore, even in the setting of a negative sestamibi scan, the majority of patients with primary HPT are still candidates for MIP.

Similar content being viewed by others
REFERENCES
Chen H, Sokoll LJ, Udelsman R. Outpatient minimally invasive parathyroidectomy: a combination of sestamibi-SPECT localization, cervical block anesthesia, and intraoperative parathyroid hormone assay. Surgery 1999; 126:1016–1021
Satchie B, Chen H. Radioguided techniques for parathyroid surgery. Asian J Surg 2005; 28:77–81
Delbridge LW, Dolan SJ, Hop TT, Robinson BG, Wilkinson MR, Reeve TS. Minimally invasive parathyroidectomy: 50 consecutive cases. Med J Aust 2000; 172:418–422
Bergenfelz A, Lindblom P, Tibblin S, Westerdahl J. Unilateral versus bilateral neck exploration for primary hyperparathyroidism: a prospective randomized controlled trial. Ann Surg 2002; 236:543–551
Udelsman R. Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann Surg 2002; 235:665–670
Bergenfelz A, Lindblom P, Tibblin S, Westerdahl J. Unilateral versus bilateral neck exploration for primary hyperparathyroidism: a prospective randomized controlled trial. Ann Surg 2002; 236:543–551
Goldstein RE, Blevins L, Delbeke D, Martin WH. Effect of minimally invasive radioguided parathyroidectomy on efficacy, length of stay, and costs in the management of primary hyperparathyroidism. Ann Surg 2000; 231:732–742
Chen H. Radioguided Parathyroid surgery. Adv Surg 2004; 38:377–392
Chen H, Mack E, Starling JR. Radioguided parathyroidectomy is equally effective for both adenomatous and hyperplastic glands. Ann Surg 2003; 238:332–337
Chen H, Pruhs Z, Starling JR, Mack E. Intraoperative parathyroid hormone testing improves cure rates in patients undergoing minimally invasive parathyroidectomy. Surgery 2005; 138:583–587
Ito F, Sipple R, Lederman J, Chen H. The utility of intraoperative bilateral internal jugular venous sampling with rapid parathyroid hormone testing. Ann Surg 2007 (in press)
Irvin GL, III, Solorzano CC, Carneiro DM. Quick intraoperative parathyroid hormone assay: surgical adjunct to allow limited parathyroidectomy, improve success rate, and predict outcome. World J Surg 2004; 28:1287–1292
Chen H, Mack E, Starling JR. A comprehensive evaluation of perioperative adjuncts during minimally invasive parathyroidectomy: which is most reliable? Ann Surg 2005; 242:375–380
Siegel A, Alvarado M, Barth RJ, Jr., Brady M, Lewis J. Parameters in the prediction of the sensitivity of parathyroid scanning. Clin Nucl Med 2006; 31:679–682
Casas AT, Burke GJ, Sathyanarayana, Mansberger AR, Jr., Wei JP. Prospective comparison of technetium-99m-sestamibi/iodine-123 radionuclide scan versus high-resolution ultrasonography for the preoperative localization of abnormal parathyroid glands in patients with previously unoperated primary hyperparathyroidism. Am J Surg 1993; 166:369–373
Haber RS, Kim CK, Inabnet WB. Ultrasonography for preoperative localization of enlarged parathyroid glands in primary hyperparathyroidism: comparison with (99m)technetium sestamibi scintigraphy. Clin Endocrinol (Oxf) 2002; 57:241–249
Frydman J, Bianco J, Drezner M, Chen H. Thallium-pertechnetate subtraction scanning in the preoperative localization of an ectopic undescended parathyroid gland. Clin Nucl Med 2004; 29:542–544
Reidel MA, Schilling T, Graf S, Hinz U, Nawroth P, Buchler MW, Weber T. Localization of hyperfunctioning parathyroid glands by selective venous sampling in reoperation for primary or secondary hyperparathyroidism. Surgery 2006; 140:907–913
Sugg SL, Fraker DL, Alexander R, Doppman JL, Miller DL, Chang R, Skarulis MC, Marx SJ, Spiegel AM, Norton JA. Prospective evaluation of selective venous sampling for parathyroid hormone concentration in patients undergoing reoperations for primary hyperparathyroidism. Surgery 1993; 114:1004–1009
Clark OH, Okerlund MD, Moss AA, Stark D, Norman D, Newton TH, Duh QY, Arnaud CD, Harris S, Gooding GA. Localization studies in patients with persistent or recurrent hyperparathyroidism. Surgery 1985; 98:1083–1094
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lal, A., Chen, H. The Negative Sestamibi Scan: Is a Minimally Invasive Parathyroidectomy Still Possible?. Ann Surg Oncol 14, 2363–2366 (2007). https://doi.org/10.1245/s10434-007-9451-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-007-9451-3