Abstract
Background
The aim of this study was to analyze the risk factors for local and distant recurrence after intersphincteric resection (ISR) for very low rectal adenocarcinoma.
Methods
One hundred twenty consecutive patients with T1–T3 rectal cancers located 1–5 (median 3) cm from the anal verge underwent ISR. Univariate and multivariate analyses of prospectively recorded clinicopathologic parameters were performed.
Results
Fifty patients had disease categorized as stage I, 21 as stage II, 46 as stage III, and 3 as stage IV on the basis of International Union Against Cancer tumor, node, metastasis staging system. Median follow-up time was 3.5 years. The 3-year rates of local and distant recurrence were 6% and 13%, respectively. Univariate analysis of the risk factors for local recurrence revealed pathologic T, pathologic stage, focal dedifferentiation, microscopic resection margins, and preoperative serum CA 19-9 level to be statistically significant. Multivariate analysis showed resection margin, focal dedifferentiation, and serum CA 19-9 level to be independently significant. Univariate analysis of the risk factors for distant recurrence indicated tumor location, combined resection, tumor annularity, pathologic N, lateral pelvic lymph node metastasis, pathologic stage, histologic grade, lymphovascular invasion, perineural invasion, and adjuvant chemotherapy to be significant. Multivariate analysis identified pathologic N, histologic grade, and tumor location to be independently significant.
Conclusion
Profiles of risk factors for local and distant recurrences after ISR are different. With local recurrence, the resection margin, focal dedifferentiation, and serum CA 19-9 level are important. For distant recurrence, the lymph node status, histologic grade, and tumor location need to be taken into account.
Similar content being viewed by others
Standard surgery for patients with massively invasive rectal adenocarcinoma located within 5 cm from the anal verge is abdominoperineal resection.1 To avoid permanent colostomy for such patients, modern intersphincteric resection (ISR) was developed in the 1980s and became well established in the 1990s.2–4 ISR is currently defined as a procedure obtaining sufficient margins by removing part or whole of the internal sphincter and restoring bowel continuity for rectal cancers involving or next to the anal canal. ISR is usually performed in combination with total mesorectal excision. Cautious performance of this operation has been reported to allow satisfactory results with regard to both defecatory function and oncologic outcome.4–7
In our previous study, we showed that ISR with meticulous dissection and irrigation after closure of the distal stump does not increase risk of local or distant recurrence.8 ISR without radiotherapy is usually sufficient for patients with T1–T2 tumors. However, with T3 tumors, neoadjuvant therapy should be considered if resection margins are estimated to be insufficient.8
Appropriate selection of patients who are at high risk for recurrence is essential to reduce unnecessary toxicity and costs of neoadjuvant and adjuvant therapy for those at low risk. Selection criteria are thus needed to stratify patients for neoadjuvant and adjuvant therapy and also for clinical trials. At present, however, there have been few studies addressing risk factors for recurrence after ISR. The aim of this study was thus to conduct retrospective exploratory analysis of the risk factors for local and distant recurrences after ISR for very low rectal adenocarcinoma.
Patients and Methods
Between October 1993 and February 2007, 122 patients with massively invasive rectal adenocarcinomas located within 5 cm from the anal verge underwent ISR at the National Cancer Center Hospital, Tokyo. Selection criteria for ISR were as follows: (1) sufficient medical fitness; (2) normal sphincter function; (3) distance between the tumor and the anorectal junction (upper edge of the surgical anal canal) of <2 cm; (4) no involvement of the external sphincter; and (5) no signs of disseminated disease. The patients were assessed with chest and abdominal computed tomography (CT), digital anorectal examination, and radiological studies, including endorectal ultrasound, thin-section helical CT, or high-resolution magnetic resonance imaging (MRI). Approval by the institutional review board was not required for the observational study. All patients gave informed consent for usage of their data for analysis.
Univariate and multivariate analyses of 26 prospectively recorded clinicopathologic variables were conducted for the 120 consecutive patients who did not receive neoadjuvant radiotherapy. Data from the remaining two given radiotherapy were excluded from the present analysis.
Surgical Procedures
The surgical procedures were described previously8 and are basically similar to those originally documented by Schiessel et al.4,7 The intersphincteric plane between the puborectalis and the internal sphincter was dissected cautiously as caudal as possible under direct vision by electrocautery. If the lower edge of the tumor was reached, the anal canal was closed just below the tumor, and then washed with povidone iodine followed by saline. A self-holding retractor was applied to the anal canal, the internal sphincter was circumferentially incised and the intersphincteric plane was dissected. A resection margin of at least 1 cm was always attempted. After removal of the rectum, the pelvic cavity and anal canal were washed, and then a coloanal anastomosis was made.
Histopathologic Examination
Results of histopathologic examination were prospectively documented in the pathology report form. Evaluated variables included gross tumor morphology, pathologic depth of transmural invasion (pT), pathologic regional lymph node metastasis (pN), pathologic lateral pelvic lymph node metastasis, pathologic distant metastasis (pM), pathologic stage, histopathologic grade, lymphovascular invasion, perineural invasion, mucin production, focal dedifferentiation, and circumferential and distal resection margins. pT, pN, pM, pathologic stage, and histopathologic grade were classified according to the International Union Against Cancer tumor, node, metastasis (TNM) classification.9 Perineural invasion was defined as the presence of cancer cells inside the perineurium.10 Focal dedifferentiation was defined as the presence of polygonal, noncolumnar cancer cells which had a single or a solitary trabecular form with indistinct polarity and had a diffusely infiltrative pattern at the invasive front.11,12
Follow-up
All of the patients were followed up with a median follow-up time of 3.5 (range, .9–11.7) years for those who remained alive, and 93 patients (78%) could be followed up for more than 2 years. Patients with stage I tumors were examined by chest and abdominopelvic CT, as well as carcinoembryonic antigen measurement every year for at least 5 years. Patients with stage II tumors were examined every 6 months for 2 years, then yearly for at least 3 years. Patients with stage III tumors were examined every 4 months for 2 years, then every 6 months for at least 3 years.
Statistical Analysis
The starting point for the recurrence-free interval was the day of surgery, and data on patients who were alive or free of recurrence were censored at the last follow-up. Local recurrence was defined as confined to the pelvis and distant recurrence as present outside of the pelvis.
Survival curves were estimated by the Kaplan-Meier method, and differences in survival were evaluated with the log rank test. Multivariate analysis was performed by Cox regression model with the forward stepwise method (likelihood ratio). All statistical analyses were conducted by SPSS for Windows, version 11.0J (SPSS-Japan, Tokyo, Japan). P values were two sided and were considered to be statistically significant at <.05.
Results
Clinicopathologic Findings
Findings for 26 clinicopathologic variables related to patient and tumor characteristics, treatment, and pathology are summarized in Table 1. There were 92 male and 28 female patients with a median age of 57 (range, 26–75) years. The median distance from the anal verge to the tumor was 3 (range, 1–5) cm.
A total of 103 patients underwent partial resection of the internal sphincter and 17 underwent complete resection. A small part of the external sphincter was resected in six patients to obtain sufficient surgical margins. All patients underwent total mesorectal excision. In addition to total mesorectal excision, 46 patients received extended lateral pelvic lymph node dissection. The median number of lymph nodes removed at surgery was 29 (range, 4–88), and 108 patients (90%) underwent dissection of 12 or more nodes. Combined resection of adjacent organs was performed for 12 patients. Two patients with a solitary liver metastasis and one with a solitary lung metastasis underwent complete resection of their metastases. A total of 108 patients had a protective stoma, which was closed 3 months after ISR. Postoperatively, 26 patients with stage III disease and 1 with curatively resected liver metastasis received adjuvant chemotherapy with 5-fluorouracil plus leucovorin, or uracil-tegafur plus leucovorin on the basis of the results from the National Surgical Adjuvant Breast and Bowel Project Protocol C-06,13 or oral uracil-tegafur on the basis of the results of the National Surgical Adjuvant Study of Colorectal Cancer 01 randomized trial.14
The median tumor size was 3.7 (range, 1–12) cm. Data on TNM classifications and histopathologic findings are provided in Table 1. Resection margins were macroscopically negative in all patients, but microscopically positive in four. One patient had both circumferential and distal positive margins, and the other three had a circumferential positive margin. Excluding these four patients, the median distal margin was 1.2 (range, .3–4) cm.
Of 39 patients (33%) who experienced complications, 30 were treated conservatively and 9 received surgery. Of 15 patients (13%) with anastomotic leakage, 6 underwent emergency operations. One patient who had anastomotic leakage and sepsis died on the third postoperative day (30-day mortality rate = .8%).
Survival and Recurrence
At the last follow-up in February 2008, 112 patients were alive and 8 were dead. Causes of death included rectal cancer (n = 4 patients), other cancers (n = 2), anastomotic leakage (n = 1), and cerebral contusion (n = 1). The estimated overall 3- and 5-year survival rates were 95% and 91%, respectively, including one hospital death.
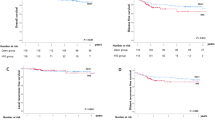
A total of 20 patients (17%) experienced recurrence. Estimated 3- and 5-year cumulative rates for overall recurrence were 17% and 23%, respectively (Fig. 1). Sites of the first recurrence included the pelvis in six patients, pelvis and lung in one, inguinal lymph nodes in two, inguinal lymph nodes and lung in one, lung in four, lung and liver in one, and liver in five. The incidences of overall recurrence for stage I, II, III, and IV disease were 5%, 22%, 27%, and 50%, respectively.
In total, eight patients (6.7%) developed local recurrence, with estimated 3- and 5-year cumulative rates of 6% and 10%, respectively (Fig. 1). Detailed sites of local failure included the internal iliac or obturator nodes in three patients, circumferential resection margin in two, anastomosis in one, seminal vesicle in one, and sacrum in one. The incidences of local failure for stage I, II, III, and IV disease were 2%, 19%, 7%, and 0%, and for pathological T1, T2, and T3 tumors were 4%, 2%, and 12%, respectively.
Estimated 3- and 5-year cumulative rates for distant recurrence, found in 15 patients (13%), were 13% and 18%, respectively (Fig. 1). The incidences of distant recurrence for stage I, II, III, and IV disease were 6%, 5%, 22%, and 33%, respectively.
Univariate Analysis
Cumulative local recurrence was statistically significantly associated with pT, pathologic stage, focal dedifferentiation, microscopic resection margins, and the preoperative serum CA 19-9 level (Table 1).
Cumulative distant recurrence was statistically significantly associated with distance of the tumor from the anal verge, combined resection, tumor annularity, pN, lateral pelvic lymph node metastasis, pathologic stage, histopathologic grade, lymphovascular invasion, perineural invasion, and adjuvant chemotherapy (Table 1).
Multivariate Analysis
Multivariate analysis was performed for those factors associating statistically significantly with cumulative local recurrence and distant recurrence on univariate analysis. The multivariate analysis of four variables, excluding pathological stage, revealed that a positive microscopic resection margin (hazard ratio, 19 [95% confidence interval, 3.3–111]; P = .001), positive focal dedifferentiation (22 [1.6–333]; P = .021), and preoperative serum CA 19-9 level of >37 U/mL (5.6 [1.1–29]; P = .04) were independently associated with an high local recurrence rate. The 3-year cumulative local recurrence rates for patients with zero, one, two, and three positive risk factors were estimated to be 0%, 8%, 29%, and 100%, respectively (Fig. 2).
Multivariate analysis for distant recurrence with seven variables, excluding pathological stage and lateral pelvic lymph node metastasis, revealed that pN1 or pN2 (hazard ratio, 13 [95% confidence interval, 3.0–53]; P < .001), poorly differentiated histology (6.4 [1.4–29]; P = .015), and distance of tumor from the anal verge less than 2.5 cm (3.7 [1.2–12]; P = .026) were independently associated with a poorer prognosis. The 3-year cumulative distant recurrence rates for patients with zero, one, and two positive risk factors were estimated to be 0%, 23%, and 40%, respectively (Fig. 3).
Discussion
In the present study, we found by univariate analysis that pT, pathologic stage, focal dedifferentiation, microscopic resection margins, and preoperative serum CA 19-9 level were statistically significantly associated with local recurrence after ISR. On multivariate analysis, resection margins, focal dedifferentiation, and serum CA 19-9 level were independently associated with local recurrence. We could stratify high-risk patients by using these three factors. With two or more factors, the 3-year local recurrence rate was estimated to be 29% or higher. Therefore, when two or more risk factors identified here become apparent, neoadjuvant chemoradiotherapy should be provided to widen resection margins, or abdominoperineal resection should be substituted for ISR.
Preoperative radiotherapy or chemoradiotherapy are generally applied as standard neoadjuvant therapy for T3 and/or lymph node positive rectal cancers in general, in addition to total mesorectal excision. This is based on evidence that radiotherapy better reduces local recurrence and prolongs disease-free and overall survival when compared with surgery alone,15,16 and that preoperative chemoradiotherapy is more effective for local control, less toxic, and more favorable for sphincter preservation than postoperative therapy.17
However, neoadjuvant and adjuvant therapy strategies to prevent local and distant recurrence after ISR have yet to be established. There is great variation in application of radiotherapy as a neoadjuvant against local recurrence, with reported rates ranging from 0% to 88%. Schiessel et al.7 never provided radiation, even for T3 tumors, like us, whereas Rullier et al.18 irradiate all T3 tumors and some T1 and T2 lesions. The other authors provided radiotherapy to 25% to 75% of patients.5,6,19,20 Although there is some dependence on selected patient population, tumor stage, and staging accuracy, usage also seems to reflect surgeons’ preferences.
Radiotherapy for rectal cancer in general is well known to have the potential to cause damage to anorectal21,22 and sexual23,24 functions. In cases with very low rectal cancer necessitating ISR, if radiation is provided, damage to the sphincter is inevitable and may be catastrophic for some patients whose sphincters are also damaged by surgery. Chamlou et al.20 reported that functional results after ISR are statistically significantly altered by preoperative radiotherapy. Ten (42%) of 24 patients who received preoperative radiotherapy of 45 Gy were incontinent as compared with 7 (15%) of 46 without radiotherapy (P = .02).20 Therefore, more selective usage of radiotherapy in case with ISR seems to be preferable than in the general rectal cancer population.
Because preoperative radiotherapy is known to be more effective and less toxic,17 it is preferable to stratify patients preoperatively. For this purpose, high-resolution MRI is accurate at estimating the resection margin status. In a prospective study of 408 rectal cancer patients, the MERCURY Study Group found that high-resolution MRI predicted a clear circumferential resection margin with an overall accuracy rate of 88%.25
Focal dedifferentiation,11,12 also known as “tumor budding,”26 can be accurately estimated by excisional or transanal submucosal biopsy26 before ISR. The transanal submucosal biopsy allows specimens to be removed from the boundary zone between the tumor and the normal mucosa, including the submucosal tissue with exploratory excisional forceps. On the basis of this technique, the submucosal invasive frontal region can be predicted with up to 86% accuracy.26
Although the exact relation between CA 19-9 and local recurrence is unclear, CA 19-9 is easily assessable. Thus, preoperative performance of high-resolution MRI, excisional/submucosal biopsy, and serum CA 19-9 measurement is recommended for every candidate for ISR and warrants further investigation and validation.
In our previous study, we observed the 3-year cumulative local recurrence rate of 0% in patients with T1–T2 tumors and thus stated that meticulous performance of ISR allows local control without radiotherapy for such lesions.8 In the present investigation, however, we found two cases (2.8%) with local recurrence. One patient with a pT1 tumor and a microscopic positive margin developed anastomotic recurrence 4.4 years after ISR. Another with a pT2 tumor had liver metastasis 10 months after ISR and underwent partial hepatectomy. This patient subsequently developed lung, liver, arm, and brain metastases, and also experienced pelvic recurrence in a seminal vesicle 2 years after ISR. Because the former case had a disease-positive surgical margin and the latter developed pelvic recurrence after fatal disseminated diseases, these two cases should be regarded as exceptional. Therefore, we still consider ISR without radiotherapy to be sufficient treatment for T1–T2 tumors in general. However, if patients have two or more of the risk factors we identified in the present study, neoadjuvant therapy should be considered.
Of the other studies on ISR, only three mentioned risk factors for local recurrence. Schiessel et al.7 reported that only Dukes' stage and the T stage had an impact on local failure. Chamlou et al.20 described overall survival to be statistically significantly influenced by pathologic TNM stage and pT on univariate analysis, but found no impact of the investigated factors on local recurrence. Analyzing data of 134 patients with rectal cancer located 2 to 11 (median 6.5) cm from the anal verge, undergoing not only ISR, but also low anterior resection or coloanal anastomosis, Paty et al.27 found that mesenteric implants, a positive microscopic resection margin, a T3 tumor, perineural invasion, blood vessel invasion, and poorly differentiated histology were statistically significantly associated with pelvic recurrence on univariate analysis. In line with the previous reports, pT and pathologic staging were identified as prognostic factors in the present study as well. In addition, these variables are regarded as category I prognostic factors.28 Therefore, they should be included with the above-mentioned list for further validation.
To our knowledge, risk factors for distant as opposed to local recurrence have hitherto not been studied separately and sufficiently. We here found that by univariate analysis, cumulative distant recurrence was statistically significantly associated with distance of tumor from the anal verge, combined resection, tumor annularity, pN, lateral pelvic lymph node metastasis, pathologic stage, histopathologic grade, lymphovascular invasion, perineural invasion, and adjuvant chemotherapy. By multivariate analysis, pathologic lymph node involvement, histologic grade, and tumor location were independently associated with distant recurrence. For patients with one or more positive risk factors, the 3-year cumulative distant recurrence rate was estimated to be 23% or higher. Because adjuvant chemotherapy for stage II and III disease is believed to reduce distant recurrence by 30% to 40%, we recommend adjuvant chemotherapy for patients with one or more risk factors, in line with other authors’ recommendations.7,18,19
As we showed, the risk factor profiles for distant and local recurrence differ, as do the prophylactic treatments. Therefore, local and distant recurrence should be analyzed separately. This is now feasible in the era of modern imaging technologies, with the availability of high-resolution MRI, multidetector row CT, and positron emission tomography-CT, which enable accurate diagnosis and differentiation of local and distant recurrence.
In conclusion, this retrospective exploratory study suggests that profiles of risk factors for local and distant recurrence after ISR may differ greatly. With local recurrence, the resection margin, focal dedifferentiation, and serum CA 19-9 level seem to be important. For distant recurrence, the lymph node status, histologic grade, and tumor location need to be taken into account. By using these factors, we may be able to stratify patients for neoadjuvant and adjuvant therapy and also for future clinical trials. These results warrant further investigation and validation with larger data sets or in future prospective trials according to the scoring system we have outlined.
References
Nicholls RJ, Hall C. Treatment of non-disseminated cancer of the lower rectum. Br J Surg 1996;83:15–8.
Basso N, Minervini S, Marcelli M. Modified abdominotransanal resection for cancer of the lower third of the rectum. Dis Colon Rectum 1987;30:641–3.
Kusunoki M, Shoji Y, Yanagi H, et al. Modified anoabdominal rectal resection and colonic J-pouch anal anastomosis for lower rectal carcinoma: preliminary report. Surgery 1992;112:876–83.
Schiessel R, Karner-Hanusch J, Herbst F, et al. Intersphincteric resection for low rectal tumors. Br J Surg 1994;81:1376–8.
Kusunoki M, Yanagi H, Shoji Y, et al. Anoabdominal rectal resection and colonic J pouch–anal anastomosis: 10 years’ experience. Br J Surg 1997;84:1277–80.
Gamagami RA, Liagre A, Chiotasso P, et al. Coloanal anastomosis for distal third rectal cancer: prospective study of oncologic results. Dis Colon Rectum 1999;42:1272–5.
Schiessel R, Novi G, Holzer B, et al. Technique and long-term results of intersphincteric resection for low rectal cancer. Dis Colon Rectum 2005;48:1858–65.
Akasu T, Takawa M, Yamamoto S, et al. Incidence and patterns of recurrence after intersphincteric resection for very low rectal adenocarcinoma. J Am Coll Surg 2007;205:642–7.
Sobin LH, Wittekind CH (International Union Against Cancer), eds. TNM Classification of Malignant Tumours, 6th edition. New York: Wiley-Liss, 2002
Fujita S, Shimoda T, Yoshimura K, et al. Prospective evaluation of prognostic factors in patients with colorectal cancer undergoing curative resection. J Surg Oncol 2003;84:127–31.
Ono M, Sakamoto M, Ino Y, et al. Cancer cell morphology at the invasive front and expression of cell adhesion-related carbohydrate in the primary lesion of patients with colorectal carcinoma with liver metastasis. Cancer 1996;78:1179–86.
Tominaga K, Nakanishi Y, Nimura S, et al. Predictive histopathologic factors for lymph node metastasis in patients with nonpedunculated submucosal invasive colorectal carcinoma. Dis Colon Rectum 2005;48:92–100.
Lembersky BC, Wieand HS, Petrelli NJ, et al. Oral uracil and tegafur plus leucovorin compared with intravenous fluorouracil and leucovorin in stage II and III carcinoma of the colon: results from National Surgical Adjuvant Breast and Bowel Project Protocol C-06. J Clin Oncol 2006;24:2059–64.
Akasu T, Moriya Y, Ohashi Y, et al. National Surgical Adjuvant Study of Colorectal Cancer Adjuvant chemotherapy with uracil-tegafur for pathological stage III rectal cancer after mesorectal excision with selective lateral pelvic lymphadenectomy: a multicenter randomized controlled trial. Jpn J Clin Oncol 2006;36:237–44.
Kapiteijn E, Marijnen CA, Nagtegaal ID, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 2001;345:638–46.
Improved survival with preoperative radiotherapy in resectable rectal cancer. Swedish rectal cancer trial. N Engl J Med 1997; 336:980–7
Sauer R, Becker H, Hohenberger W, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 2004;351:1731–40.
Rullier E, Laurent C, Bretagnol F, et al. Sphincter-saving resection for all rectal carcinomas: the end of the 2-cm distal rule. Ann Surg 2005;241:465–9.
Saito N, Moriya Y, Shirouzu K, et al. Intersphincteric resection in patients with very low rectal cancer: a review of the Japanese experience. Dis Colon Rectum 2006; 49(10 Suppl):S13–22
Chamlou R, Parc Y, Simon T, et al. Long-term results of intersphincteric resection for low rectal cancer. Ann Surg 2007;246:916–21.
Peeters KC, van de Velde CJ, Leer JW, et al. Late side effects of short-course preoperative radiotherapy combined with total mesorectal excision for rectal cancer: increased bowel dysfunction in irradiated patients–a Dutch Colorectal Cancer Group Study. J Clin Oncol 2005;23:6199–206.
Pollack J, Holm T, Cedermark B, et al. Long-term effect of preoperative radiation therapy on anorectal function. Dis Colon Rectum 2006;49:345–52.
Marijnen CA, van de Velde CJ, Putter H, et al. Impact of short-term preoperative radiotherapy on health-related quality of life and sexual functioning in primary rectal cancer: report of a multicenter randomized trial. J Clin Oncol 2005;23:1847–58.
Heriot AG, Tekkis PP, Fazio VW, et al. Adjuvant radiotherapy is associated with increased sexual dysfunction in male patients undergoing resection for rectal cancer: a predictive model. Ann Surg 2005;242:502–11.
MERCURY Study Group. Diagnostic accuracy of preoperative magnetic resonance imaging in predicting curative resection of rectal cancer: prospective observational study. BMJ 2006; 333:779
Ueno H, Mochizuki H, Shinto E, et al. Histologic indices in biopsy specimens for estimating the probability of extended local spread in patients with rectal carcinoma. Cancer 2002;94:2882–91.
Paty PB, Enker WE, Cohen AM, et al. Treatment of rectal cancer by low anterior resection with coloanal anastomosis. Ann Surg 1994;219:365–73.
Compton CC, Fielding LP, Burgart LJ, et al. Prognostic factors in colorectal cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med 2000;124:979–94.
Acknowledgments
Supported in part by a Grant-in-Aid for Clinical Research for Evidence Based Medicine, a Grant-in-Aid for Cancer Research from the Ministry of Health, Labor and Welfare, and a grant from the Foundation for Promotion of Cancer Research in Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akasu, T., Takawa, M., Yamamoto, S. et al. Intersphincteric Resection for Very Low Rectal Adenocarcinoma: Univariate and Multivariate Analyses of Risk Factors for Recurrence. Ann Surg Oncol 15, 2668–2676 (2008). https://doi.org/10.1245/s10434-008-0047-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-008-0047-3