Abstract
Background
Pelvic radiotherapy (RT) is a standard component of the management for patients with locally advanced rectal cancer or squamous cell carcinoma of the anus. Pelvic RT leads to permanent and irreversible ovarian failure in young women. This study aimed to determine the effectiveness of robotically assisted laparoscopic ovarian transposition (OT) before RT in women with rectal or anal cancer who wanted to preserve normal ovarian function.
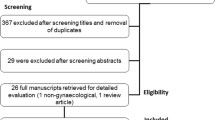
Methods
The study reviewed the medical records of all patients treated at our institution from August 2009 to October 2014 who received robotically assisted laparoscopic OT for rectal or anal cancer before RT. Clinical and hormonal data were abstracted to determine ovarian function.
Results
The study identified 22 women with rectal (n = 20) or anal (n = 2) cancer. The median age of the women was 39 years (range 26–45 years). For one patient, OT was technically not feasible. The postoperative course was uneventful in all but one case. Follow-up data on ovarian function were unavailable for 3 patients. The median times from RT initiation to the last gynecologic or hormonal evaluation were 9 months (range 5–47 months) and 10.5 months (range 5–47 months), respectively. At the last gynecologic or hormonal follow-up visit, ovarian function was preserved in 12 (67%) of 18 evaluable patients, including 9 (90%) of 10 patients 40 years of age or younger and 3 (38%) of 8 patients older than 40 years (P = 0.07).
Conclusions
Robotically assisted laparoscopic bilateral OT is safe and can lead to preservation of ovarian function in two-thirds of patients with low gastrointestinal cancer undergoing pelvic RT. It should be considered in this setting, especially for women age 40 years or younger, to avoid premature menopause and its associated sequelae.
Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66:7–30.
Inra JA, Syngal S. Colorectal cancer in young adults. Dig Dis Sci. 2015;60:722–33.
Meyer JE, Narang T, Schnoll-Sussman FH, Pochapin MB, Christos PJ, Sherr DL. Increasing incidence of rectal cancer in patients aged younger than 40 years: an analysis of the surveillance, epidemiology, and end results database. Cancer. 2010;116:4354–9.
Bailey CE, Hu CY, You YN, et al. Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975–2010. JAMA Surg. 2015;150:17–22.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology. 2016. https://www.nccn.org/professionals/physician_gls/f_guidelines.asp. Accessed 16 Jun 2016.
Joseph DA, Miller JW, Wu X, et al. Understanding the burden of human papillomavirus-associated anal cancers in the U. S. Cancer. 2008;113(10 Suppl):2892–900.
Nelson RA, Levine AM, Bernstein L, Smith DD, Lai LL. Changing patterns of anal canal carcinoma in the United States. J Clin Oncol. 2013;31:1569–75.
O’Connell JB, Maggard MA, Liu JH, Etzioni DA, Livingston EH, Ko CY. Do young colon cancer patients have worse outcomes? World J Surg. 2004;28:558–62.
Quah HM, Joseph R, Schrag D, et al. Young age influences treatment but not outcome of colon cancer. Ann Surg Oncol. 2007;14:2759–65.
Gunderson LL, Winter KA, Ajani JA, et al. Long-term update of US GI intergroup RTOG 98-11 phase III trial for anal carcinoma: survival, relapse, and colostomy failure with concurrent chemoradiation involving fluorouracil/mitomycin versus fluorouracil/cisplatin. J Clin Oncol. 2012;30:4344–51.
Torrealday S, Pal L. Premature menopause. Endocrinol Metab Clin N Am. 2015;44:543–57.
Wan J, Gai Y, Li G, Tao Z, Zhang Z. Incidence of chemotherapy- and chemoradiotherapy-induced amenorrhea in premenopausal women with stage II/III colorectal cancer. Clin Colorectal Cancer. 2015; 14:31–4.
Bisharah M, Tulandi T. Laparoscopic preservation of ovarian function: an underused procedure. Am J Obstet Gynecol. 2003;188:367–70.
Loren AW, Mangu PB, Beck LN, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31:2500–10.
Society of Gynecologic Oncology. SGO clinical practice statement: salpingectomy for ovarian cancer prevention, 2013. https://www.sgo.org/clinical-practice/guidelines/sgo-clinical-practice-statement-salpingectomy-for-ovarian-cancer-prevention. Accessed 16 Jun 2016.
Wo JY, Viswanathan AN. Impact of radiotherapy on fertility, pregnancy, and neonatal outcomes in female cancer patients. Int J Radiat Oncol Biol Phys. 2009;73:1304–12.
Vassilakopoulou M, Boostandoost E, Papaxoinis G, de La Rouge TM, Khayat D, Psyrri A. Anticancer treatment and fertility: effect of therapeutic modalities on reproductive system and functions. Crit Rev Oncol Hematol. 2016;97:328–34.
Wallace WH, Thomson AB, Kelsey TW. The radiosensitivity of the human oocyte. Hum Reprod. 2003;18:117–21.
Meirow D, Nugent D. The effects of radiotherapy and chemotherapy on female reproduction. Hum Reprod Update. 2001;7:535–43.
Wallace WH, Thomson AB, Saran F, Kelsey TW. Predicting age of ovarian failure after radiation to a field that includes the ovaries. Int J Radiat Oncol Biol Phys. 2005;62:738–44.
Spanos CP, Mamopoulos A, Tsapas A, Syrakos T, Kiskinis D. Female fertility and colorectal cancer. Int J Colorectal Dis. 2008;23:735–43.
O’Neill MT, Ni Dhonnchu T, Brannigan AE. Topic update: effects of colorectal cancer treatments on female fertility and potential methods for fertility preservation. Dis Colon Rectum. 2011;54:363–9.
Azem F, Amit A, Merimsky O, Lessing JB. Successful transfer of frozen-thawed embryos obtained after subtotal colectomy for colorectal cancer and before fluorouracil-based chemotherapy. Gynecol Oncol. 2004;93:263–5.
Marhhom E, Cohen I. Fertility preservation options for women with malignancies. Obstet Gynecol Surv. 2007;62:58–72.
Levi M, Shalgi R, Brenner B, et al. The impact of oxaliplatin on the gonads: from bedside to the bench. Mol Hum Reprod. 2015;21:885–93.
Cercek A, Siegel CL, Capanu M, Reidy-Lagunes D, Saltz LB. Incidence of chemotherapy-induced amenorrhea in premenopausal women treated with adjuvant FOLFOX for colorectal cancer. Clin Colorectal Cancer. 2013;12:163–7.
Tulandi T, Al-Took S. Laparoscopic ovarian suspension before irradiation. Fertil Steril. 1998;70:381–3.
Elizur SE, Tulandi T, Meterissian S, Huang JY, Levin D, Tan SL. Fertility preservation for young women with rectal cancer: a combined approach from one referral center. J Gastrointest Surg. 2009;13:1111–5.
Kurt M, Uncu G, Cetintas SK, Kucuk N, Guler S, Ozkan L. Successful spontaneous pregnancy in a patient with rectal carcinoma treated with pelvic radiotherapy and concurrent chemotherapy: the unique role of laparoscopic lateral ovary transposition. Eur J Gynaecol Oncol. 2007;28:408–10.
Al-Badawi IA, Al-Aker M, AlSubhi J, et al. Laparoscopic ovarian transposition before pelvic irradiation: a Saudi tertiary center experience. Int J Gynecol Cancer. 2010;20:1082–6.
Al-Asari S, Abduljabbar A. Laparoscopic ovarian transposition before pelvic radiation in rectal cancer patient: safety and feasibility. Ann Surg Innov Res. 2012;6:9.
Barahmeh S, Al Masri M, Badran O, et al. Ovarian transposition before pelvic irradiation: indications and functional outcome. J Obstet Gynaecol Res. 2013;39:1533–7.
Treissman MJ, Miller D, McComb PF. Laparoscopic lateral ovarian transposition. Fertil Steril. 1996;65:1229–31.
Gomez-Hidalgo NR, Darin MD, Dalton H, et al. Ovarian torsion after laparoscopic ovarian transposition in patients with gynecologic cancer: a report of two cases. J Minim Invasive Gynecol. 2015;22:687–90.
Picone O, Aucouturier JS, Louboutin A, Coscas Y, Camus E. Abdominal wall metastasis of a cervical adenocarcinoma at the laparoscopic trocar insertion site after ovarian transposition: case report and review of the literature. Gynecol Oncol. 2003;90:446–9.
van Beurden M, Schuster-Uitterhoeve AL, Lammes FB. Feasibility of transposition of the ovaries in the surgical and radiotherapeutical treatment of cervical cancer. Eur J Surg Oncol. 1990;16:141–6.
Hwang JH, Yoo HJ, Park SH, et al. Association between the location of transposed ovary and ovarian function in patients with uterine cervical cancer treated with (postoperative or primary) pelvic radiotherapy. Fertil Steril. 2012;97:1387–93. e1–2.
Soda I, Ishiyama H, Ono S, et al. Assessment of transposed ovarian movement: how much of a safety margin should be added during pelvic radiotherapy? J Radiat Res. 2015;56:354–9.
Acknowledgement
This study was funded in part through the NIH/NCI Support Grant P30 CA008748.
Disclosure
There are no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sioulas, V.D., Jorge, S., Chern, JY. et al. Robotically Assisted Laparoscopic Ovarian Transposition in Women with Lower Gastrointestinal Cancer Undergoing Pelvic Radiotherapy. Ann Surg Oncol 24, 251–256 (2017). https://doi.org/10.1245/s10434-016-5650-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5650-0