Abstract
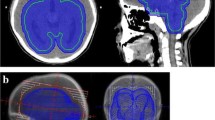
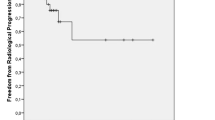
To our knowledge, there are no published reports on the effectiveness of radiosurgery in the management of brain metastases from testicular nonseminomatous germ cell tumor. The authors evaluate the results of gamma knife (GK) treatment in three patients with these unusual intracranial lesions. Between April 1995 and July 2001, three patients with brain metastasis from testicular nonseminomatous germ cell tumor underwent adjuvant radiosurgery at our department. The primary tumor had been surgically removed in all cases. At diagnosis, one patient was stage IB and two were stage III poor risk. Chemotherapy and whole brain radiotherapy were administered before radiosurgery in all cases. Pre-GK radiotherapy was administered with a daily fraction dosage of 1.8–2.0 Gy. The indications for radiosurgery were tumor volume <20 cm3, microsurgery too risky, refusal of surgery. All the lesions were located in eloquent brain areas. Post-GK high-dose chemotherapy with autologous peripheral-blood stem-cell rescue was administered in two cases due to systemic recurrence of the disease. All patients are still alive with a median and mean follow-up period after radiosurgery of 63 and 68.3 mo, respectively. They had no neurological deficits at the latest examination. Neuroradiological follow-up invariably showed tumor growth control (complete response in two cases and partial response in one) with typically delayed post-radiosurgical imaging changes (transient in two cases and long-lasting in one). In conclusion, GK seems to be highly effective and safe in brain metastases from testicular nonseminomatous germ cell tumor. In cases with diffuse metastatic brain involvement, the whole brain radiotherapy preceding radiosurgery should be delivered with ≤1.8 Gy daily fraction to prevent the risk of long-lasting post-radiosurgical imaging changes.
Similar content being viewed by others
References
Gerosa M, et al. Gamma knife radiosurgery for brain metastases: a primary therapeutic option. J Neurosurg 2002; 97 (Suppl 5):515–524.
Hasegawa T, Kondziolka D, Flickinger JC, Lunsford LD. Stereotactic radiosurgery for brain metastases from gastrointestinal tract cancer. Surg Neurol 2003; 60:506–514.
Hasegawa T, Kondziolka D, Flickinger JC, Germanwala A, Lunsford LD. Brain metastases treated with radiosurgery alone: an alternative to whole brain radiotherapy? Neurosurgery 2003; 52:1318–1326.
Jawahar A, et al. Gamma knife surgery in the management of brain metastases from lung carcinoma: a retrospective analysis of survival, local tumor control, and freedom from new brain metastasis. J Neurosurg 2004; 100:842–847.
Mingione V, Oliveira M, Prasad D, Steiner M, Steiner L. Gamma surgery for melanoma metastases in the brain. J Neurosurg 2002; 96:544–551.
Muacevic A, Kreth FW, Tonn JC, Wowra B. Stereotactic radiosurgery for multiple brain metastases from breast carcinoma. Cancer 2004; 100:1705–1711.
Nicolato A, et al. Multiple brain metastases from “lymphoepithelioma-like” thymic carcinoma: a combined stereotacticradiosurgical approach. Surg Neurol 2001; 55:232–234.
Sneed PK, et al. A multi-institutional review of radiosurgery alone vs. radiosurgery with whole brain radiotherapy as the initial management of brain metastases. Int J Radiat Oncol Biol Phys 2002; 53:519–526.
Gaspar L, et al. Recursive partitioning analysis (RPA) of prognostic factors in three radiation therapy oncology group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 1997; 37:745–751.
De Angelis LM, Yahalom J, Thaler HT, Kher U. Combined modality therapy for primary CNS lymphoma. J Clin Oncol 1992; 10:635–643.
Elisevich K, Ratkewicz A, Lownie S. Radiosurgery of deep arteriovenous malformations of the brain. Neurosurgery Quarterly 1999; 9:33–48.
Lunsford LD, Kondziolka D, Flickinger JC. Stereotactic radiosurgery for arteriovenous malformations of the brain. J Neurosurg 1991; 75:512–524.
Nataf F, et al. Parenchymal chenges after radiosurgery of cerebral arteriovenous malformations. Preliminary report of a proposed classification. Stereotact Funct Neurosurg 1997; 69:143–146.
Lunsford LD, Flickinger J, Lindner G, Maitz A. Stereotactic radiosurgery of the brain using the first United States 201 cobalt-60 source gamma knife. Neurosurgery 1989; 24:151–159.
Brown PD, Brown CA, Pollock BE, Gorman DA, Foote RL. Stereotactic radiosurgery for patients with “radioresistant” brain metastases. Neurosurgery 2002; 51:656–665.
Sheehan JP, Sun MH, Kondziolka D, Flickinger J, Lunsford LD. Radiosurgery in patients with renal cell carcinoma metastasis to the brain: long-term outcomes and prognostic factors influencing survival and local tumor control. J Neurosurg 2003; 98:342–349.
Delarive J, De Tribolet N. Métastases cérébrales, étuded’un collectif chirurgical de 81 cas. Neurochirurgie 1992; 38:89–97.
Williams SD, Einhorn LH. Brain metastases in disseminated germinal neoplasms. Incidence and clinical course. Cancer 1979; 44:1514–1516.
Cohn DA, Stuart-Harris R. Isolated central nervous system relapse of non-seminomatous germ cell tumour of the testis. A case report and review of the literature. Oncology 2001; 61:184–188.
Jelsma RK, Carroll M. Brain metastasis from nonseminomatous germ cell tumors of the testis: case report and review of the role of surgery. Neurosurgery 1989; 25:814–819.
Salvati M, et al. Solitary cerebral metastasis from tumor of the testis: some observations about treatment in two cases. Ital J Neurol Sci 1997;18:173–175.
Yoshida S, Morii K. Brain metastasis from germinal tumors of the testis. Case report. J Neurosurg 1998;88:761–763.
Gerl A, Clemm C, Kohl P, Schalhorn A, Wilmanns W. Central nervous system as sanctuary site of relapse in patients treated with chemotherapy for metastatic testicular cancer. Clin Exp Metastasis 1994;12:226–230.
Mahalati K, Bilen CY, Ozen H, Aki FT, Kendi S. The management of brain metastasis in nonseminomatous germ cell tumours. BJU Int 1999;83:457–461.
Guenot M, Wager M, Bataille B, Irani J, Lapierre F. Métastases cérébrales des cancers testiculaires. A propos de deux cas et revue de la litérature. Neurochirurgie 1994;40:135–137.
Bokemeyer C, et al. Treatment of brain metastases in patients with testicular cancer. J Clin Oncol 1997;15:1449–1454.
Spears WT, Morphis JG II, Lester SG, Williams SD, Einhorn LH. Brain metastases and testicular tumors: long-term survival. Int J Radiat Oncol Biol Phys 1992;22:17–22.
Raina V, et al. Brain metastasis as the site of relapse in germ cell tumour of testis. Cancer 1993;72:2182–2185.
Lester SG, et al. Brain metastases and testicular tumors: need for aggressive therapy. J Clin Oncol 1984;2:1397–1403.
Logothetis CJ, Sakuels ML, Trinade A. The management of brain metastases in germ cell tumors. Cancer 1982;49:12–18.
Duchesne G, Peckham MJ. Chemotherapy and radiotherapy in advanced testicular nonseminoma. Results of treatment. Radiother Oncol 1984;1:207–215.
Peckham MJ, Barret A. The radiotherapy of testicular tumours. In: Peckham, MJ (ed). The management of testicular tumours. Edward Arnolds, Ltd: London, 1981, pp. 174–201.
Dueland S, et al. Treatment and outcome of patients with extragonadal germ cell tumours—the Norwegian Radium Hospital’s experience 1979–94. Br J Cancer 1998;77:329–335.
Lunsford LD, Kondziolka D, Maitz A, Flickinger JC. Black holes white dwarfs and supernovas: imaging after radiosurgery. Stereotact Funct Neurosurg 1998; 70(Suppl):2–10.
Chitapanarux I, et al. Prospective study of stereotactic radiosurgery without whole brain radiotherapy in patients with four or less brain metastases: incidence of intracranial progression and salvage radiotherapy. J Neurooncol 2003;61:143–149.
Takahashi M, et al. Stereotactic radiosurgery (SRS) for multiple metastatic brain tumors: effects of the number of target tumors on exposure dose in normal brain tissues. Int J Clin Oncol 2003;8:289–296.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nicolato, A., Ria, A., Foroni, R. et al. Gamma knife radiosurgery in brain metastases from testicular tumors. Med Oncol 22, 45–56 (2005). https://doi.org/10.1385/MO:22:1:045
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1385/MO:22:1:045