Abstract
We have recently developed an associative Brain-Computer Interface (BCI) for neuromodulation in chronic and acute stroke patients that leads to functional improvements. The control signal is the movement related cortical potential (MRCP) that develops prior to movement execution. The MRCP increases in variability as a novel task is learned, which in turn significantly decreases the detection accuracy. In the current study we sought to investigate if tactile stimulation, often implemented in rehabilitation, may act as a primer to our associative BCI by decreasing MRCP variability. Six chronic stroke patients were exposed to one session of tactile stimulation, and the MRCP of an arm lifting task, repeated 30 times, extracted. Results reveal that for three patients the MRCP detection accuracy expressed as the rate of true and false positives was improved. In two patients however the detection accuracy declined while one patient was unable to complete the experiment. Since tactile stimulation is a common tool implemented by physiotherapists to train patients to perform dynamic movements with the appropriate muscle pattern to avoid compensatory actions by other muscles it will be important to decipher why it results in such differential effects across patients.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
- Brain-computer-interface
- Movement-related-cortical potential
- Stroke
- Tactile stimulation training
- Detection accuracy
1 Introduction
A brain-computer-interface (BCI) designed for neuromodulation uses brain signals to control an external device without the conventional way of nerves and muscles [1, 2]. In previous studies we have shown significant improvements in the functionality of chronic and subacute stroke patients exposed to a novel associative BCI intervention [3, 4]. Patients were able to walk faster and increase their foot tapping frequency significantly following only three sessions of training [4]. We also reported significant plasticity induction at the level of the motor cortex using non-invasive transcranial magnetic stimulation [4, 5]. In this associative BCI, the reorganization of brain areas, necessary to re-learn motor tasks after brain damage, is enhanced by establishing a causal relationship between the patient’s intention (interpreted with the BCI) and the artificial reproduction of the intended movement.
The rationale of this relies on the concept of associative brain plasticity, i.e., the reinforcement of cortical connections due to the coupling of efferent (brain command) and afferent signals (signals from the body generated during motion and sent to the brain along nerves) [5,6,7]. The associative BCI system interprets the patient’s intention in terms of the movement to be executed and controls an electrical stimulation system, which artificially reproduces the intended movement in the target limb by delivering electrical current to the peripheral nerves. This approach, based on animal and human studies [8, 9] creates a strong causal connection between the intention to move expressed by the brain and the sensation of movement which arrives at the brain with afferent activity from the limb.
In these studies the control signal was the movement related cortical potential (MRCP). The MRCP is a slow negative potential that starts to develop approximately one to two seconds prior to movement onset, attains its largest amplitude just prior to movement onset, followed by a re-afferent phase [10]. The MRCP generated following a cue to the user comprises several well defined parts, which are known to be linked to specific neurophysiological mechanisms [11]. The first deflection, the early MRCP, commences immediately following the warning stimulus [12]. The late MRCP appears 1 to 0.5 s prior to the cue to perform the movement [12], is associated to the planning of voluntary movements and is altered in neurological disease [13]. During the movement execution and after the cue, a more complex waveform may be observed thought to be related to somatosensory feedback and the attention level during task execution [12].
Depending on the lesion site and the extend of the lesion, stroke patients generally exhibit a variable MRCP shape between trials and days although the time of peak negativity remains stable at least in chronic stroke patients [4] when referenced to a cue that indicates the patient to perform the movement. However, since the ultimate goal of our associative BCI is to provide high detection accuracy and thus a maximal number of precisely timed pairings of the MRCP and the artificially generated afferent signal, the trial to trial variability of the MRCP is problematic. Specifically as the algorithm is required to detect movement intent prior to the movement execution phase.
Clinicians attempt to restore normal functionality by using a variety of techniques to train the patient to react to external stimuli appropriately and as fast as possible. The main aim is to provide the patient with the correct way of executing the movement. One of these involves tactile stimulation that guides patients through initiation and completion of intended tasks. In the current study we investigated if such tactile stimulation may be used as a primer for our associative BCI intervention by training patients to execute the task in a similar manner. We hypothesized that the MRCP associated to the task becomes more stable following the tactile stimulation training, thus improving detection accuracy and consequently performance of our BCI algorithm.
2 Methods
2.1 Patients
Six patients at least one year post the injury (age of 18–35 mean 27.5 years) provided informed consent and agreed to participate in the study. Inclusion criteria were: 1. 18 years of age or above, 2. Ischemic stroke at least 12 month prior to the study, 3. Able to follow commands, 4. Ability to be active for at least one hour, 5. Able to voluntarily elevate the affected arm by a minimum of 5 cm (elbow) and 30 cm (hand). The patients were all affected on the left side of the brain due to an ischemic stroke. Table 1 provides patient demographics.
2.2 Movement Related Cortical Potential (MRCP)
Nine channels of monopolar EEG were recorded using an active EEG electrode system and g.USBamp amplifier (gTec, GmbH, Austria) from F3, FC5, FC1, T7, C3, Cz, Cp5, CP1 and P3 according to the standard international 10–20 system. The ground and reference electrodes were placed on Fz and the left earlobe, respectively. Impedance was maintained below 5 KΩ. Signals were filtered from 0 to 100 Hz and sampled at 256 Hz. A single channel of surface electromyography (EMG) was recorded from the right deltoid muscle to control for the subject’s movement. The electrodes (Ambu Neuroline 720, Ag/AgC1) were placed parallel on the skin at the frontal aspect of the affected deltoid muscle.
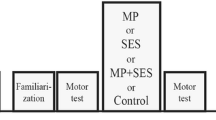
Patients were asked to attempt to lift their arm contralateral to the lesion site 30 times. The patient set-up and position is depicted in Fig. 1A. A custom made Matlab script provided visual information via a screen positioned 2 m in front of the patient on when to mentally prepare, execute, and release the movement (Fig. 1B). The visual cue was comprised of five phases defined as focus, preparation, execution, hold and rest time. After a random duration to focus, a ramp appeared on the screen. A cursor moved along the ramp and when it reached the upward turn, the movement period commenced and patients had to perform and sustain a shoulder elevation while placing the lower arm and hand onto a pillow placed on their lap, followed by a rest period. A total of 30 trials were completed prior to and following the intervention. Patients were instructed to attempt to perform the movement as fast as possible when the cursor had reached the upwards turn and to maintain the new position for 2 s, following which they relaxed again 4–5 s prior to the next cue being provided.
Experimental set-up. (A) Patient set-up and position during the session. (B) The visual display shown to the patients during the single trials. FOCUS appeared on the screen initially followed by the schematic of a step-function. Subjects were required to start the movement once the moving cursor (triangle) reached the upward slope. The word REST appeared last on the screen.
2.3 Feature Extraction from the MRCP
EEG data were divided into epochs of 4 s (from 2 s before to 2 s after the visual cue) for each movement, band pass-filtered from 0.05 Hz to 10 Hz, and subsequently a Laplacian channel [14] was used, to enhance the MRCP in each epoch. A window of 500 ms on either side of task onset was chosen and if any epoch’s peak negativity was outside the selected window it was discarded. This was to ensure that any mistrials where the patient commenced the movement too early or too late were not included in the final analysis. In addition, epochs containing eye-induced artifacts such as eye movements, eye blinks or extra-ocular muscle activity (Electrooculographic (EOG) activity) exceeding 125 µV were also discarded. Based on these remaining epochs, the mean peak negativity of the MRCP (PN) was defined as the time of occurrence of the minimum value of the averaged MRCP in relation to the visual cue. In addition the variability of the signal in the time of −1 to −0.5 ms prior to cue onset was extracted.
2.4 Tactile Stimulation Training
The tactile stimulation training commenced with a five minute massage and deep pressure application to the Flexor Retinaculum of the hand and the insertion point of the Biceps Brachii and Brachialis. These muscles were chosen as they were identified by the therapist of the patients as being the primary muscles limiting the task initiation and completion. This first phase of the training is intended to provide the patient with additional sensory input to the weak muscles so as to facilitate their activation in the next phase. In phase two, patients were asked to perform the task of elevating the shoulder and placing their affected arm onto a pillow located in front of them (Fig. 1A). The patients were instructed to initiate and start the movement, and if required, the therapist provided additional assistance to ensure the movement could be completed. In case the patient did not commence the movement, the therapist held the grip on the patient’s lower arm, providing periodic deep pressure as additional sensory input (Fig. 2). Patients completed on average five trials. The total duration of the training did not exceed 20 min.
2.5 MRCP Detection
Movement detection parameters were extracted from the EEG epochs using the Locality Preserving Projection (LPP) method followed by a linear discriminant analyses (LDA) classifier (LPP-LDA). The details of this technique are provided elsewhere [15]. The detection latency (DL) was defined as the difference between the movement detection time and the real movement onset as calculated from the EMG signals. The true positive rate (TPR) was defined as the number of true detections divided by the total true events. The false positive rate (FPR) was defined as the number of false detections divided by the number of total events. TPR and FPR were used as the detection features.
3 Results
An example of single trial MRCPs and the average MRCP across all electrode locations prior to the tactile stimulation training is depicted in Fig. 3. The single trials show greater variability compared to post tactile stimulation training (Fig. 4).
One patient was excluded from further analysis as this patient was unable to complete the entire experiment. For the remaining patients, an MRCP variability curve was calculated from individual pre and post training trials and the variability extracted within [−2 0] prior to movement onset. An example of the average MRCP and the associated variability curve for the single trials from one patient is shown in Fig. 5. The tactile stimulation training induced decreases in variability across patients (34–88%), however two patients exhibited large increases in variability (334 and 213%) thus the overall result was not significant.
Across all patients, the MRCP was detected at −254 ms (minus indicating prior to movement onset) and −262 ms before and following training respectively. The robustness of the detection algorithm was expressed as the rate of true positives (TPR) and false positives (FP) as a percentage. Prior to the training, these were: TPR: 51–85, FP: 16–45; and immediately following the training: TPR: 50–92, FP: 12–33. Due to the low patient numbers, no statistical comparisons were made (Table 2).
4 Discussion
In the current study we investigated the effects of adjuvant tactile stimulation tailored to guide patients through initiation and completion of the main task, on the variability of the MRCP. Three of the patients, had a decreased variability of the MRCP and concomitant improvements in detection accuracy, while in two patients the variability increased. The results in this small patient cohort indicate that for at least some patients, tactile stimulation training may be a primer to reduce MRCP variability and thus to enhance detection performance in an online associative BCI.
BCIs designed for neuromodulation attempt to restore motor function in individuals that have suffered from a central nervous system lesion such as a stroke [4, 16,17,18,19,20,21,22,23,24]. In these studies there are several control signals that are typically extracted from the ongoing EEG signals such as event related desynchronization/synchronization (ERDs and ERSs) [19, 20, 22,23,24], Mu rhythm [18] and the MRCP [4]. In all these BCI systems, it is necessary to train the detection algorithm prior to the actual BCI intervention. However, especially in ERD/ERS controlled BCIs the patients themselves also have to be trained to control the relevant brain signals where frequently 15 or more sessions are required [25, 26]. MRCP based BCIs on the other hand may be implemented from the first session as all patients are able to produce this signal modality.
The MRCP extracted from the EEG signal has several advantageous properties; 1. It can be recorded reliably from BCI naïve participants upon first time BCI use [3, 4]; 2. A relatively low number of channels is required for accurate detection [30]; 3. It can be detected prior to movement execution [31]. What is not known is how these signals change as the patient starts to recover. In studies on learning new skills in healthy subjects it is known that the area responsible for controlling specific muscles increases [27] and specific areas increase their response to artificial stimuli such as TMS [28]. As such it is expected that in stroke patients both in the chronic and the acute phase, similar changes may occur.
Recently we have shown that the MRCP is significantly affected by learning of a novel motor task as well as attention changes of the user [29]. Specifically the variability within the preparation phase is affected and it is this, which the detection algorithm is trained on. Since the associative BCI when implemented as part of the rehabilitation of stroke patients will lead to significant plasticity [3, 4], it is likely that the MRCP will increase in variability much like the learning of the novel task. This however may be viewed as a positive development and algorithms that can adapt to this new state of the user will have to be developed. However, an additional problem is posed when patients are unable to reliably repeat the specific task within the BCI. This may be related to the time of task execution (patients may vary in their response time to the cue provide from trial to trial) or the recruitment patterns of muscles (patients are unable to perform the movement appropriately due to variability in the pattern of muscle activation). Here, techniques that provide the patient with immediate feedback as to the task performance may aid in reducing task variability and as a consequence MRCP variability. Tactile sensory stimulation as applied in the current study, guides the patient by providing such feedback. Data from at least three patients suggest that it may be a useful technique in some patients to improve detection accuracy, though it remains to be investigated why some patients remain unresponsive.
References
Wolpaw, J.R.: Brain-computer interfaces. Handb. Clin. Neurol. 110, 67–74 (2013)
Wolpaw, J.R., Wolpaw, E.W.: Brain-Computer Interfaces - Principles and Practice. Oxford University Press, New York (2012)
Mrachacz-Kersting, N., Stevenson, A., Aliakbaryhosseinabadi, S., Lundgaard, A., Jørgensen, H., Severinsen, K., Farina, D.: An associative brain-computer-interface for acute stroke patients. In: International Conference on Neurorehabilitation, p. 248 (2016)
Mrachacz-Kersting, N., Jiang, N., Stevenson, A.J., Niazi, I.K., Kostic, V., Pavlovic, A., Radovanovic, S., Djuric-Jovicic, M., Agosta, F., Dremstrup, K., Farina, D.: Efficient neuroplasticity induction in chronic stroke patients by an associative brain-computer interface. J. Neurophysiol. 115, 1410–1421 (2016)
Mrachacz-Kersting, N., Kristensen, S.R., Niazi, I.K., Farina, D.: Precise temporal association between cortical potentials evoked by motor imagination and afference induces cortical plasticity. J. Physiol. 590, 1669–1682 (2012)
Cooke, S.F., Bliss, T.V.P.: Plasticity in the human central nervous system. Brain 129, 1659–1673 (2006)
Stefan, K., Kunesch, E., Cohen, L.G., Benecke, R., Classen, J.: Induction of plasticity in the human motor cortex by paired associative stimulation. Brain 123, 572–584 (2000)
Bliss, T.V.P., Lomo, T.: Long-lasting potentiation of synaptic transmission in the dentate area of the anaesthetized rabbit following stimulation of the perforant path. J. Physiol. (Lond.) 232, 331–356 (1973)
Mrachacz-Kersting, N., Fong, M., Murphy, B.A., Sinkjaer, T.: Changes in excitability of the cortical projections to the human tibialis anterior after paired associative stimulation. J. Neurophysiol. 97, 1951–1958 (2007)
Kornhuber, H.H., Deecke, L.: Changes in the brain potential in voluntary movements and passive movements in man: readiness potential and reafferent potential. Pflugers Arch. Gesamte Physiol. Menschen. Tiere. 284, 1–17 (1965)
Walter, W.G., Cooper, R., Aldridge, V.J., McCallum, W.C., Winter, A.L.: Contingent negative variation: an electric sign of sensorimotor association and expectancy in the human brain. Nature 203, 380–384 (1964)
Hamano, T., Luders, H.O., Ikeda, A., Collura, T.F., Comair, Y.G., Shibasaki, H.: The cortical generators of the contingent negative variation in humans: a study with subdural electrodes. Electroencephalogr. Clin. Neurophysiol./Evoked Potentials Sect. 104, 257–268 (1997)
Ikeda, A., Shibasaki, H., Kaji, R., Terada, K., Nagamine, T., Honda, M., Kimura, J.: Dissociation between contingent negative variation (CNV) and Bereitschaftspotential (BP) in patients with parkinsonism. Electroencephalogr. Clin. Neurophysiol. 102, 142–151 (1997)
McFarland, D.J., McCane, L.M., David, S.V., Wolpaw, J.R.: Spatial filter selection for EEG-based communication. Electroencephalogr. Clin. Neurophysiol. 103, 386–394 (1997)
Xu, R., Jiang, N., Lin, C., Mrachacz-Kersting, N., Dremstrup, K., Farina, D.: Enhanced low-latency detection of motor intention from EEG for closed-loop brain-computer interface applications. IEEE Trans. Biomed. Eng. 61, 288–296 (2014)
Daly, J.J., Cheng, R., Rogers, J., Litinas, K., Hrovat, K., Dohring, M.: Feasibility of a new application of noninvasive brain computer interface (BCI): a case study of training for recovery of volitional motor control after stroke. J. Neurol. Phys. Ther. 33, 203–211 (2009)
Ang, K.K., Guan, C., Chua, K.S., Ang, B.T., Kuah, C., Wang, C., Phua, K.S., Chin, Z.Y., Zhang, H.: Clinical study of neurorehabilitation in stroke using EEG-based motor imagery brain-computer interface with robotic feedback. In: Conference Proceedings of IEEE Engineering in Medicine and Biology Society, vol. 2010, pp. 5549–5552 (2010)
Broetz, D., Braun, C., Weber, C., Soekadar, S.R., Caria, A., Birbaumer, N.: Combination of brain-computer interface training and goal-directed physical therapy in chronic stroke: a case report. Neurorehabil. Neural Repair 24, 674–679 (2010)
Cincotti, F., Pichiorri, F., Arico, P., Aloise, F., Leotta, F., de Vico Fallani, F., Millan Jdel, R., Molinari, M., Mattia, D.: EEG-based brain-computer interface to support post-stroke motor rehabilitation of the upper limb. In: Conference Proceedings of IEEE Engineering in Medicine and Biology Society, vol. 2012, pp. 4112–4115 (2012)
Li, M., Liu, Y., Wu, Y., Liu, S., Jia, J., Zhang, L.: Neurophysiological substrates of stroke patients with motor imagery-based brain-computer interface training. Int. J. Neurosci. 124, 403–415 (2014)
Young, B.M., Nigogosyan, Z., Nair, V.A., Walton, L.M., Song, J., Tyler, M.E., Edwards, D.F., Caldera, K., Sattin, J.A., Williams, J.C., Prabhakaran, V.: Case report: post-stroke interventional BCI rehabilitation in an individual with preexisting sensorineural disability. Front. Neuroeng. 7, 18 (2014)
Mukaino, M., Ono, T., Shindo, K., Fujiwara, T., Ota, T., Kimura, A., Liu, M., Ushiba, J.: Efficacy of brain-computer interface-driven neuromuscular electrical stimulation for chronic paresis after stroke. J. Rehabil. Med. 46, 378–382 (2014)
Ramos-Murguialday, A., Broetz, D., Rea, M., Laer, L., Yilmaz, O., Brasil, F.L., Liberati, G., Curado, M.R., Garcia-Cossio, E., Vyziotis, A., Cho, W., Agostini, M., Soares, E., Soekadar, S., Caria, A., Cohen, L.G., Birbaumer, N.: Brain-machine interface in chronic stroke rehabilitation: a controlled study. Ann. Neurol. 74, 100–108 (2013)
Pichiorri, F., Morone, G., Petti, M., Toppi, J., Pisotta, I., Molinari, M., Paolucci, S., Inghilleri, M., Astolfi, L., Cincotti, F., Mattia, D.: Brain-computer interface boosts motor imagery practice during stroke recovery. Ann. Neurol. 77, 851–865 (2015)
Buch, E., Weber, C., Cohen, L.G., Braun, C., Dimyan, M.A., Ard, T., Mellinger, J., Caria, A., Soekadar, S., Fourkas, A., Birbaumer, N.: Think to move: a neuromagnetic brain-computer interface (BCI) system for chronic stroke. Stroke 39, 910–917 (2008)
Kai, K.A., Cuntai, G., Sui Geok Chua, K., Beng-Ti, A., Kuah, C., Chuanchu, W., Kok, S.P., Zheng, Y.C., Haihong, Z.: A clinical study of motor imagery-based brain-computer interface for upper limb robotic rehabilitation. In: Annual International Conference of IEEE, Engineering in Medicine and Biology Society, EMBC 2009, pp. 5981–5984 (2009)
Pascual-Leone, A., Nguyet, D., Cohen, L.G., Brasil-Neto, J.P., Cammarota, A., Hallett, M.: Modulation of muscle responses evoked by transcranial magnetic stimulation during the acquisition of new fine motor skills. J. Neurophysiol. 74, 1037–1045 (1995)
Perez, M.A., Lungholt, B.K.S., Nyborg, K., Nielsen, J.B.: Motor skill training induces changes in the excitability of the leg cortical area in healthy humans. Exp. Brain Res. 159, 197–205 (2004)
Mrachacz-Kersting, N., Jiang, N., Aliakbaryhosseinabadi, S., Xu, R., Petrini, L., Lontis, R., Dremstrup, K., Farina, D.: The changing brain: bidirectional learning between algorithm and user. In: Guger, C., Allison, B.Z., Edlinger, G. (eds.) Brain-Computer Interface Research: A State-of-the-Art Summary-4. Springer, Heidelberg (2015)
Jochumsen, M., Niazi, I.K., Rovsing, H., Rovsing, C., Nielsen, G.A.R., Andersen, T.K., Dong, N.P.T., Sørensen, M.E., Mrachacz-Kersting, N., Jiang, N., Farina, D., Dremstrup, K.: Detection of movement intentions through a single channel of electroencephalography. In: Jensen, W., Andersen, O., Akay, M. (eds.) Replace, Repair, Restore, Relieve – Bridging Clinical and Engineering Solutions in Neurorehabilitation, pp. 465–472. Springer, Cham (2014)
Niazi, I.K., Mrachacz-Kersting, N., Jiang, N., Dremstrup, K., Farina, D.: Peripheral electrical stimulation triggered by self-paced detection of motor intention enhances motor evoked potentials. IEEE Trans. Neural Syst. Rehabil. Eng 20, 595–604 (2012)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this paper
Cite this paper
Mrachacz-Kersting, N., Aliakbaryhosseinabadi, S., Pedersen, M., Jiang, N., Farina, D. (2017). Tactile Stimulation Training to Enhance MRCP Detection in Chronic Stroke Patients. In: Schmorrow, D., Fidopiastis, C. (eds) Augmented Cognition. Enhancing Cognition and Behavior in Complex Human Environments. AC 2017. Lecture Notes in Computer Science(), vol 10285. Springer, Cham. https://doi.org/10.1007/978-3-319-58625-0_26
Download citation
DOI: https://doi.org/10.1007/978-3-319-58625-0_26
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-58624-3
Online ISBN: 978-3-319-58625-0
eBook Packages: Computer ScienceComputer Science (R0)