Abstract
The ongoing pandemic of COVID-19 is a global challenge which resulted in significant morbidity and mortality worldwide. It has also adversely affected the economy and social integrity. There is rising concern about the mental health challenges of the general population, COVID-19-infected patients, close contacts, elderly, children and health professionals. This chapter focusses on various mental health challenges during the COVID-19 pandemic.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
16.1 Introduction
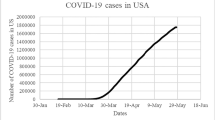
There is a major health crisis going on in the world currently. A newly emerged zoonotic viral infection known as novel coronavirus disease (COVID-19) is affecting people, globally taking the form of a pandemic. Over the past few months, there is a significant increase in mortality and morbidity due to this pandemic. Till date (29 March 2020), there are more than 680,000 total cases with 31,920 deaths, 146,396 recovered over 202 countries (COVID-19 Coronavirus Pandemic 2020). As per the situation report of the World Health Organization (WHO), by the end of 28 March 2020, more than half of the global deaths and infected cases were from the European region (World Health Organization 2020a). As the disease is spreading in a rapid pace, most of the affected countries are not able to meet the demands of the personal protective equipment (PPE) and infrastructure requirement (World Health Organization 2020a). At the current stage, the major objectives laid by the WHO are prevention of human-to-human transmission, limiting the spread of infection to close contacts and medical professionals, preventing the development of complications in infected persons, isolation and quarantine facility provision, availing diagnostic and laboratory facility, research to produce specific treatment and vaccine and minimizing the socioeconomic impact on the community (World Health Organization 2020a). It has been noticed over the past few months that during this outbreak of COVID-19 infection, there are increasing mental health issues among the general population, elderly, children, migrant workers and healthcare professionals other than the patients with COVID-19 infection (Duan and Zhu 2020; Chen et al. 2020; Liem et al. 2020; Yang et al. 2020a, b). To date there are no specific recommendations from international bodies regarding addressing the mental health issues during this COVID-19 pandemic.
16.2 Impact of COVID-19 in Society
The global impact of COVID-19 has been profound, and the public health threat due to this is the most serious seen since the 1918 H1N1 influenza pandemic. The overall case fatality rate of COVISD-19 was 2.3% in China and could be variable in different countries (Novel Coronavirus Pneumonia Emergency Response Epidemiology Team 2020; Livingston and Bucher 2020). A nationwide analysis done in China showed that comorbidities are present in around one-fourth of patients with COVID-19 and predispose to poorer clinical outcomes (Novel Coronavirus Pneumonia Emergency Response Epidemiology Team 2020). The impact of the disease is beyond mortality, and morbidity has become apparent since the outbreak of the pandemic. A large population throughout the world is certain to have a massive psychological impact as evidenced by a preliminary report from China where among 1210 respondents more than half of the respondents rated the psychological impact as moderate-to-severe and about one-third reported moderate-to-severe anxiety (Wang et al. 2020a). Studies post-SARS pandemic or post-Ebola indicate that even after recovering physically from the disease, individuals suffered from social and psychological problems and similar could be the impact with this pandemic (Bobdey and Ray 2020). Evidence suggests that vulnerable groups who are confined to their homes during a pandemic can have negative health outcomes. Children especially become physically less active and have much longer screen time, irregular sleep patterns and less favourable diets, resulting in weight gain and a loss of cardiorespiratory fitness (Wang et al. 2020b). Also, there are other direct and indirect implications of the closure of schools like unintended childcare obligations, which are particularly large in healthcare occupations (Bayham and Fenichel 2020). This could be related to the current situation in most of the countries throughout the world not only in child care but also in the adult and geriatric population (Heckman et al. 2020).
COVID-19 is a supply shock and a demand shock. Both the aspects will impact on aggregate trade flow (Baldwin and Tomiura 2020). It has both direct and indirect economic implications. The stocks and flow of physical and financial assets are interrupted. An increase in health budget and a lowering of overall GDP is sure to impact the whole world (McKibbin and Fernando 2020). Another area of impact would be travel and tourism. In the current scenario, the travel of any citizen of any country has been virtually been stopped. Also, even once the pandemic is over, it is almost certain to take a long time before people become confident of travel (Anzai et al. 2020; Dinarto et al. 2020).
Stigma and fear are other aspects of the outbreak of a pandemic. It can present major barriers against healthcare seeking, social marginalization, distrust in health authorities and distortion of public perceptions of risk, resulting in mass panic among citizens and the disproportionate allocation of healthcare resources by politicians and health professionals (Barrett and Brown 2008).
Impact on the sports and other mass gatherings throughout the world cannot be ignored (Gallego et al. 2020). Within weeks of the emergence of this pandemic in China, there have been circulation of misinformation, misleading rumours and conspiracy theories about the origin paired with fear mongering, racism and compulsive buying and stocking of goods and face masks. This can be attributed to impact the social media has created (Depoux et al. 2020). Over all the pandemic will have impact in all domains of the current world starting from health, society and economy and would also impact the future policy making at global, regional and country level (Djalante et al. 2020).
16.3 Emerging Mental Health Issues in COVID-19 Pandemic
The COVID-19 pandemic is a global emergency situation while the diagnosis of specific disorders needs a specific time period which is a major constraint to quantify the mental health issues. Moreover, many of the survivors may develop mental disorders long after the event. Therefore, multiple and complex confounding variables makes the issue hazy. Fortunately, studies evaluating the mental health issue have been coming out gradually which needs more time certainly to get replicable findings.
16.3.1 Among General Population
As the COVID-19 pandemic has been spreading rapidly across the globe, the foremost mental health issue has raised the level of stress or anxiety expressed in public mental health term (Dong and Bouey 2020). Inadequate knowledge regarding the incubation period of the virus, route of transmission, treatment and safety measures cause fear and anxiety (Li et al. 2020; Ho et al. 2020; Goyal et al. 2020). The locked-down state bounds residents to become homebound which causes negative mental health outcomes like anxiety states and insecurity regarding the future (Li et al. 2020). The citizens also feel monotony, disappointment and irritability under the locked-down state (Ho et al. 2020). One study reported severe and wide spectrum mental health impacts of the pandemic (Goyal et al. 2020). The event can precipitate new mental disorders and exacerbate the previously present disorders (Goyal et al. 2020). The general population can experience fear and anxiety of being sick or dying, helplessness, blame the people who are already affected and precipitate the mental breakdown (Goyal et al. 2020). A wide range of psychiatric disorders can be found such as depressive disorders, anxiety disorders, panic disorder, somatic symptoms, self-blame, guilt, posttraumatic stress disorder (PTSD), delirium, psychosis and even suicide (Goyal et al. 2020; Yi et al. 2020).
16.3.2 Among COVID-19 Cases
The suspected and/or confirmed COVID-19 persons largely experience fear regarding the high contagiousness and fatality (Wang et al. 2020a; Li et al. 2020). The quarantined people feel boredom, loneliness, anger, depression, anxiety, denial, despair, insomnia, harmful substance use, self-harm and suicidality (Wang et al. 2020a; Dong and Bouey 2020; Li et al. 2020; Yi et al. 2020). The survivors are the high-risk people to develop a wide range of mental disorders such as depression, anxiety and PTSD (World Health Organization 2020a). As a continuation of safety behaviours, patients may develop obsessive-compulsive disorder (OCD) (Li et al. 2020). Moreover, physical symptoms of COVID-19 such as fever, hypoxia and cough along with adverse effects of prescribed medications (corticosteroids) may cause more anxiety and mental distress (Wang et al. 2020a). A recent study of 1210 participants from 194 cities in China reported that 53.8% had a moderate or severe psychological impact, 31.3% had some sort of depression, 36.4% had some sort of anxiety and 32.4% had some sort of stress (Liu et al. 2020). Poor or very poor self-rated health status was significantly associated with a greater psychological impact of the COVID-19 (Liu et al. 2020).
16.3.3 Among Family Members and Close Contacts
Along with the persons with COVID-19, the family members and close contacts face psychological problems as they have been traced, isolated or quarantined which makes people anxious and guilty regarding the aftermath of the contagion, quarantine and stigma on their family members and friends (Wang et al. 2020a). The family members who lose their loved ones from the pandemic results in anger and resentment (Goyal et al. 2020). Furthermore, they also feel shame, guilt or stigma for those family members who are sick and/or quarantined, and some studies reported PTSD and depression among the family members and close contacts (Goyal et al. 2020). On the other hand, the children who have been isolated or quarantined during the pandemic have higher chances to develop acute stress disorder, adjustment disorder and grief (Shah et al. 2020). PTSD was reported among 30% of the children and early loss of or separation from parents during childhood also has long-term adverse effects on mental health, including higher chances of developing mood disorders, psychosis and suicidality (Shah et al. 2020).
16.3.4 Among Healthcare Workers
As pandemics are the global public mental health emergency, healthcare services demand increases sharply. Furthermore, many countries do not have adequate manpower as well as resources to cope with COVID-19. Thus, healthcare providers have to face an increased workload with the fear of being infected. Many times, they have been quarantined frequently when they contact COVID-19-confirmed persons.
Increased workload, isolation and discrimination are common which result in physical exhaustion, fear, emotional disturbance and sleep disorders (Ho et al. 2020). A recent study involving 1563 health professionals reported that more than half (50.7%) of the participants reported depressive symptoms, 44.7% anxiety and 36.1% sleep disturbance (Ho et al. 2020). Moreover, there are not adequate services to provide counselling and psychiatric screening services for anxiety, depression and suicidality for physicians who have been dealing with infected persons (World Health Organization 2020b). It is also meaningful to postulate that many physicians develop PTSD, depression, anxiety and burnout after the cessation of the pandemic (World Health Organization 2020b). Along with the physicians, the frontline healthcare providers (FHCP) can develop mental disorders such as depression, anxiety and PTSD (Li et al. 2020). Previous articles reported that FHCP (paramedics, ambulance personnel and healthcare workers) have also shown heightened stress and emotional disturbances and have higher levels of depression and anxiety (Goyal et al. 2020).
This is estimated as the chances of getting infected is much higher with the risk of exposure which creates a fear of transmission to their loved ones and children. Furthermore, the conflict professionalism and personal fear for oneself causes burnouts and physical and mental symptoms (Goyal et al. 2020).
16.3.5 Among Special Population (Old Age and Co-morbidities)
As this pandemic has been spreading rapidly across the world, it is bringing a considerable degree of fear, worry and concern among few certain groups particularly, in older adults and people with underlying comorbid disorders (Dong and Bouey 2020). It has a potential impact on the existing diseases, and the affected persons may lead to psychiatric symptoms which possibly related to the interplay of mental disorders and immunity (World Health Organization 2020b). The symptoms of COVID-19 can also worsen cognitive distress and anxiety among people who have poor mental capabilities previously (World Health Organization 2020b).
Patients with pre-existing severe mental illness (SMI) have been inevitably affected by the pandemic (Ho et al. 2020). In-patients, especially those requiring long-term hospitalization in closed wards, pose a high risk of cluster contagion. Due to traffic restrictions and isolation measures, outpatients with SMI are facing difficulties to receive maintenance treatment and may thus end up with mental relapse and uncontrollable situations (Ho et al. 2020). Patients with chronic physical illness (e.g., chronic renal failure, diabetes mellitus and cardio-cerebrovascular diseases) also need regular follow-up in hospitals which become problematic and raise the chances of deterioration.
16.4 Coping with Mental Health Issues During COVID-19 Pandemic
While the healthcare sector and government officials from all over the world is focusing on the control of the pandemic adopting various preventive strategies, there is little attention provided to the mental health status of the isolated, panicked and house-arrested people. Due to lack of regular social activities and staying at home for a longer time will impact their emotional well-being. Research has also shown that sudden outbreak can worsen the mental health conditions of those with pre-existing mental health illness (Ho et al. 2020).
To avoid a distressing situation, individuals should not get exposed to media coverage too much, to maintain a healthy relationship, get in touch with friends and family members on a regular interval using social media and start thinking positively (CDC 2020). If coronavirus anxiety shows up, try to share the fear with others, which will calm the fear, and also try to increase self-awareness by getting adequate sleep, exercising regularly and employing different relaxation techniques (Kecmanovic 2020). As recommended by Ho et al. (2020) in this era of technology, healthcare services can introduce providing online psychological support services for those individuals who lost their close relatives due to COVID-19 (Ho et al. 2020). To support the morale and mental health of the frontline healthcare professionals, healthcare organizations should introduce shorter working periods, regular breaks and rotating shifts (Ho et al. 2020). People can cope with the mental health challenges by adopting various lifestyle-related measures (Figs. 16.1 and 16.2).
16.5 Myths and Facts About COVID-19
During a new infectious disease outbreak, a great deal of uncertainty remains from the pattern of transferring, risk factors involved and prevention and treatment (Schuchat et al. 2011). Rumours and myths create more panic among the general public as they are malevolent in nature and can alter people’s observations towards the disease. The world is witnessing the same for the new public health crises with the emergence and spread of 2019 novel coronavirus. When the disease originated from Wuhan city of China, it was declared as a second-class infectious disease, but most of the areas of the country adopted the first level of response measure to control, and the measures were taken has no scientific basis and no effective outcomes were recorded after applying those measures by the China government (Xiao and Torok 2020).
The virus cannot be killed by cold and snow, and it can be transmitted in areas with hot and humid climate (WHO 2020). People of all age groups are susceptible to get infected with COVID-19. Elderly people with underlying health conditions such as diabetes, heart disease and asthma are more vulnerable (Fong 2020). Although there is no significant number of paediatric cases so far, children are vulnerable to the infection (Hong et al. 2020), and to date, there is no evidence of vertical transmission of this infection (Baud et al. 2020).
Several national and international newspapers, tabloids and media channels all over the world are reporting that the smokers are prone to catch coronavirus infection due to weakened lungs and will put the smokers at risk (Mullin 2020). However, a recent systematic review finding revealed that no significant association is found between active smoking and the severity of COVID 19 (Lippi and Henry 2020).
There are reports of using oseltamivir, lopinavir/ritonavir, prednisone, antibiotics, and traditional Chinese medicine for the treatment of patients with COVID-19. Again, there is no scientific evidence to support that they will be effective against COVID-19 apart from scrupulous personal care such as the use of personal protection precaution to reduce the risk of transmission, early diagnosis, isolation and supportive treatments for affected patients (Xiao and Torok 2020; Wang et al. 2020c).
There is also some misconception among the general people that by taking hot bath, people will not get infected with the infection or spraying alcohol or chlorine all over the body can kill the infection (WHO 2020). Proper public health information should be provided, based on scientific research to general people to reduce stress and anxiety, otherwise it will be difficult to implement control measures.
16.6 Precautionary Measures and Recommendations
No definite treatment is available for the treatment of the COVID-19 infection. Prevention is the best strategy to combat the COVID-19 pandemic. Prevention is not a difficult task as it is commonly thought to be. For the effective prevention of COVID-19, broadly two types of precautionary measures to be taken, as mentioned below:
-
1.
General precautionary measures (Fig. 16.3): It is meant for everybody in the community.
-
2.
Specific precautionary measures (Fig. 16.4): It is meant for persons who are sick, close contacts of COVID-19, travellers and healthcare workers.
Broadly, there are three groups of population as mentioned below:
-
(a)
General population
-
(b)
COVID-19 cases and close contacts
-
(c)
Healthcare workers
The precautions and recommendations are targeted to address the needs of the above three groups of the population. Prevailing myths and unawareness about precautionary measures may cause distress among people. There is a need to follow certain recommendations for effective coping with mental health challenges (Table 16.1).
Individuals who experience psychological distress must report or inform their difficulties, rather than hiding them. Individuals who experience persistence distress may seek help from the mental health professionals through helplines available or in hospitals in cases of emergency situations. Figures 16.5 and 16.6 summarize the recommendations according the risk severity and management approach to mental health difficulties during COVID-19 pandemic, respectively.
16.7 Conclusions
COVID-19 carries significant mental health hazards. There is a paucity of research addressing the mental health issues during the COVID-19 pandemic. As the mortality and morbidity statistics are reaching new peaks every day, isolation and lockdown states are getting prolonged, recreational opportunities for people are lessened and the financial crisis is building in, mental health issues are likely to grow exponentially. There is a need to understand the mental perspectives of COVID-19 and possible measures to cope with the pandemic for their effective management.
16.8 Future Perspectives
The mental health issues associated with the COVID-19 pandemic can be immediate (short-term) or remote (long-term). Existing literature addresses the immediate mental health concerns only. It is important to see the long-term mental health sequels of COVID-19 infection. Earlier pieces of evidence suggest that maternal exposure to influenza infection during the epidemic of influenza in Europe increased the risk of schizophrenia in offspring, possibly by altering the neurodevelopmental process (Mednick et al. 1988; Murray et al. 1992). Similarly, childhood exposure to measles may later result in the development of subacute sclerosing panencephalitis (SSPE) (Campbell et al. 2007). Nothing is known about the after-effects of novel coronavirus infection; hence, there is a need for extensive research in terms of its impact on various groups of populations (pregnant, young children, adults and other vulnerable populations).
Similarly, it is required to understand the mental healthcare needs of patients with COVID-19, close contacts, health professionals dealing with COVID-19 patients and the general population. Future research should also consider the feasibility and efficacy of various online psychotherapeutic interventions during the COVID-19 pandemic, globally with a specific focus in the low- and middle-income countries (LMICs). As there is a concern about contacting infection during direct contact with patients, online consultation can be a potential mode of delivering therapy (Greenhalgh et al. 2020).
Executive Summary
-
Mental health issues differ among various populations during the COVID-19 pandemic.
-
Vulnerable populations like COVID-19 cases, close contacts, elderly, children and health professionals are expected to have more difficulties with coping.
-
Appropriate precautionary measures may reduce the psychological distress.
-
Myths associated with COVID-19 may also lead to distress and inappropriate lifestyle measures.
-
People experiencing distress should adopt various healthy relaxation measures and if required help from mental health professionals.
References
Anzai A, Kobayashi T, Linton NM, Kinoshita R, Hayashi K, Suzuki A et al (2020) Assessing the impact of reduced travel on exportation dynamics of novel coronavirus infection (COVID-19). J Clin Med 9(2):601
Baldwin R, Tomiura E (2020) 5 Thinking ahead about the trade impact of COVID-19. Econ Time COVID-19. 59
Barrett R, Brown PJ (2008) Stigma in the time of influenza: social and institutional responses to pandemic emergencies. J Infect Dis 197(Suppl 1):S34–S37
Baud D, Giannoni E, Pomar L, Qi X, Nielsen-Saines K, Musso D et al (2020) COVID-19 in pregnant women—authors’ reply. Lancet Infect Dis. https://doi.org/10.1016/S1473-3099(20)30192-4
Bayham J, Fenichel EP (2020) The impact of school closure for COVID-19 on the US Healthcare Workforce and the Net Mortality Effects. medRxiv. 2020.03.09.20033415
Bobdey S, Ray S (2020) Going viral–Covid-19 impact assessment: a perspective beyond clinical practice. J Mar Med Soc 22(1):9
Campbell H, Andrews N, Brown KE, Miller E (2007) Review of the effect of measles vaccination on the epidemiology of SSPE. Int J Epidemiol 36(6):1334–1348
CDC (2020) Mental health and coping during COVID-19. http://adultmentalhealth.org/mental-health-and-coping-during-covid-19/. Cited 29 Mar 2020
Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L et al (2020) Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 7(4):e15–e16
COVID-19 Coronavirus Pandemic (2020). https://www.worldometers.info/coronavirus/. Cited 29 Mar 2020
Depoux A, Martin S, Karafillakis E, Bsd RP, Wilder-Smith A, Larson H (2020) The pandemic of social media panic travels faster than the COVID-19 outbreak. J Travel Med. https://doi.org/10.1093/jtm/taaa031
Dinarto D, Wanto A, Sebastian LC (2020) Global health security – COVID-19: impact on Bintan’s tourism sector. https://dr.ntu.edu.sg//handle/10356/137356. Cited 29 Mar 2020
Djalante R, Shaw R, DeWit A (2020) Building resilience against biological hazards and pandemics: COVID-19 and its implications for the Sendai Framework. Prog Disaster Sci 6:100080
Dong L, Bouey J (2020) Public mental health crisis during COVID-19 pandemic, China. Emerg Infect Dis 26(7). https://doi.org/10.3201/eid2607.200407
Duan L, Zhu G (2020) Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry 7(4):300–302
Fong LY (2020) Frequently asked questions and myth busters on COVID-19. https://worldwide.saraya.com/about/news/item/frequently-asked-questions-and-myth-busters-on-covid-19. Cited 29 Mar 2020
Gallego V, Nishiura H, Sah R, Rodriguez-Morales AJ (2020) The COVID-19 outbreak and implications for the Tokyo 2020 Summer Olympic Games. Travel Med Infect Dis:101604
Goyal K, Chauhan P, Chhikara K, Gupta P, Singh MP (2020) Fear of COVID 2019: first suicidal case in India. Asian J Psychiatry 49:e101989
Greenhalgh T, Wherton J, Shaw S, Morrison C (2020) Video consultations for covid-19. BMJ 368:m998
Heckman GA, Saari M, McArthur C, Wellens NI, Hirdes JP (2020) RE: COVID-19 response and chronic disease management. https://www.cmaj.ca/content/re-covid-19-response-and-chronic-disease-management. Cited 29 Mar 2020
Ho CS, Chee CY, Ho RC (2020) Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singap 49(1):1
Hong H, Wang Y, Chung H-T, Chen C-J (2020) Clinical characteristics of novel coronavirus disease 2019 (COVID-19) in newborns, infants and children. Pediatr Neonatol. https://doi.org/10.1016/j.pedneo.2020.03.001
Kecmanovic J (2020) 7 science-based strategies to cope with coronavirus anxiety. The Conversation. http://theconversation.com/7-science-based-strategies-to-cope-with-coronavirus-anxiety-133207. Cited 30 Mar 2020
Li W, Yang Y, Liu Z-H, Zhao Y-J, Zhang Q, Zhang L et al (2020) Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci 16(10):1732–1738
Liem A, Wang C, Wariyanti Y, Latkin CA, Hall BJ (2020) The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiatry 7(4):e20
Lippi G, Henry BM (2020) Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19). Eur J Intern Med. https://doi.org/10.1016/j.ejim.2020.03.014
Liu JJ, Bao Y, Huang X, Shi J, Lu L (2020) Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolesc Health. https://www.thelancet.com/journals/lanchi/article/PIIS2352-4642(20)30096-1/abstract. Cited 30 Mar 2020
Livingston E, Bucher K (2020) Coronavirus disease 2019 (COVID-19) in Italy. JAMA. https://jamanetwork.com/journals/jama/fullarticle/2763401. Cited 29 Mar 2020
McKibbin WJ, Fernando R (2020) The global macroeconomic impacts of COVID-19: seven scenarios. Social Science Research Network, Rochester, NY. Report No.: ID 3547729. https://papers.ssrn.com/abstract=3547729. Cited 29 Mar 2020
Mednick SA, Machon RA, Huttunen MO, Bonett D (1988) Adult schizophrenia following prenatal exposure to an influenza epidemic. Arch Gen Psychiatry 45(2):189–192
Mullin G (2020) SMOKE SCREEN Smoking ‘may increase risk of catching coronavirus’ and worsen symptoms, scientists warn. https://www.thesun.co.uk/news/11098194/smoking-increase-coronavirus-risk-worsen-symptoms/. Cited 29 Mar 2020
Murray RM, Jones P, O’Callaghan E, Takei N, Sham P (1992) Genes, viruses and neurodevelopmental schizophrenia. J Psychiatr Res 26(4):225–235
Novel Coronavirus Pneumonia Emergency Response Epidemiology Team (2020) [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China]. Zhonghua Liu Xing Bing Xue Za Zhi Zhonghua Liuxingbingxue Zazhi 41(2):145–151
Schuchat A, Bell BP, Redd SC (2011) The science behind preparing and responding to pandemic influenza: the lessons and limits of science. Clin Infect Dis 52(Suppl 1):S8–S12. https://academic.oup.com/cid/article/52/suppl_1/S8/498182. Cited 30 Mar 2020
Shah K, Kamrai D, Mekala H, Mann B, Desai K, Patel RS (2020) Focus on mental health during the coronavirus (COVID-19) pandemic: applying learnings from the past outbreaks. Cureus 12(3). https://www.cureus.com/articles/29485-focus-on-mental-health-during-the-coronavirus-covid-19-pandemic-applying-learnings-from-the-past-outbreaks. Cited 30 Mar 2020
Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS et al (2020a) Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 17(5):1729
Wang G, Zhang Y, Zhao J, Zhang J, Jiang F (2020b) Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 395(10228):945–947
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J et al (2020c) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. https://doi.org/10.1001/jama.2020.1585
WHO (2020) Coronavirus disease (COVID-19) advice for the public: myth busters. World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters. Cited 29 Mar 2020
World Health Organization (2020a) Coronavirus disease 2019 (COVID-19) situation report—68. World Health Organization. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200328-sitrep-68-covid-19.pdf?sfvrsn=384bc74c_2. Cited 29 Mar 2020
World Health Organization (2020b) Mental health and COVID-19. http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/novel-coronavirus-2019-ncov-technical-guidance/coronavirus-disease-covid-19-outbreak-technical-guidance-europe/mental-health-and-covid-19. Cited 30 Mar 2020
Xiao Y, Torok ME (2020) Taking the right measures to control COVID-19. Lancet Infect Dis. https://doi.org/10.1016/S1473-3099(20)30152-3
Yang Y, Li W, Zhang Q, Zhang L, Cheung T, Xiang Y-T (2020a) Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry 7(4):e19
Yang P, Liu P, Li D, Zhao D (2020b) Corona Virus Disease 2019, a growing threat to children? J Infect. https://doi.org/10.1016/j.jinf.2020.02.024
Yi Y, Lagniton PN, Ye S, Li E, Xu R-H, Zhong B-L et al (2020) COVID-19: what has been learned and to be learned about the novel coronavirus disease. Int J Biol Sci 16(10):1753–1766
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 The Editor(s) (if applicable) and The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Kar, S.K., Yasir Arafat, S.M., Kabir, R., Sharma, P., Saxena, S.K. (2020). Coping with Mental Health Challenges During COVID-19. In: Saxena, S. (eds) Coronavirus Disease 2019 (COVID-19). Medical Virology: From Pathogenesis to Disease Control. Springer, Singapore. https://doi.org/10.1007/978-981-15-4814-7_16
Download citation
DOI: https://doi.org/10.1007/978-981-15-4814-7_16
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-4813-0
Online ISBN: 978-981-15-4814-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)