Abstract
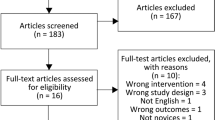
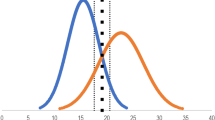
This paper describes transfer of skills obtained from training with the EyeSI virtual reality simulator of ophthalmic surgery to real-life surgical performance. Skills in real-life phacoemulsification surgery were assessed by systematic blinded evaluation of surgical videos based on the OSACCS system. Nineteen Danish cataract surgeons with varying clinical experience levels had their cataract surgery skills evaluated before and after completing a standardized mastery learning program on the EyeSI. It was found that transfer of skills could be demonstrated only for surgeons with a real-life experience of less than 75 completed, independent cases. We could not demonstrate transfer of skills from the EyeSI cataract module to the EyeSI vitreoretinal module, so each subspecialty seems to require specific training. Finally, the discriminative power of EyeSI simulation between emerging surgeons and experts was found to reside only in the first training sessions. The EyeSI simulator in its current state of development, and our implementation of it, seems to require further development before it can be used as a tool to select residents for surgical training and to re-certify more senior surgeons.




Similar content being viewed by others
References
Birkmeyer JD, Finks JF, O'Reilly A, Oerline M, Carlin AM, Nunn AR, Dimick J et al (2013) Surgical skill and complication rates after bariatric surgery. N Engl J Med 369:1434–1442. https://doi.org/10.1056/NEJMsa1300625
Hajari JN, Christensen U, Kiilgaard JF, Bek T, la Cour M (2015) Reoperation for rhegmatogenous retinal detachment as quality indicator for disease management: a register study. Acta Ophthalmol 93:505–511. https://doi.org/10.1111/aos.12756
Heimann H, Bornfeld N, Bartz-Schmidt UK, Hilgers RD, Heussen N (2009) Einfluss des Operateurs auf die Operationsergebnisse bei rhegmatogener Ablatio retinae im Rahmen der “Scleral Buckling versus Primary Vitrectomy in Rhegmatogenous Retinal Detachment Study” (Anaylsis of the surgeon factor in the treatment results of rhegmatogenous retinal detachment in the “Scleral Buckling versus Primary Vitrectomy in Rhegmatogenous Retinal Detachment Study”). Klin Monatsbl Augenheilkd 226:991–998. https://doi.org/10.1055/s-0028-1109873
Kasotakis G, Lakha A, Sarkar B, Kunitake H, Kissane-Lee N, Dechert T, McAneny D et al (2014) Trainee participation is associated with adverse outcomes in emergency general surgery: an analysis of the National Surgical Quality Improvement Program database. Ann Surg 260:483–490. https://doi.org/10.1097/SLA.0000000000000889
Thomsen AS, Subhi Y, Kiilgaard JF, la Cour M, Konge L (2015) Update on simulation-based surgical training and assessment in ophthalmology: a systematic review. Ophthalmology 122:1111–1130. https://doi.org/10.1016/j.ophtha.2015.02.028
Tolsgaard MG, Ringsted C, Rosthoj S, Norgaard L, Moller L, Freiesleben NC, Dyre L et al (2017) The effects of simulation-based transvaginal ultrasound training on quality and efficiency of care: a multicenter single-blind randomized trial. Ann Surg 265:630–637. https://doi.org/10.1097/SLA.0000000000001656
Koch F, Koss MJ, Singh P, Naser H (2009) Virtual reality in ophthalmology. Klin Monbl Augenheilkd 226:672–676. https://doi.org/10.1055/s-0028-1109383
Lowry EA, Porco TC, Naseri A (2013) Cost analysis of virtual-reality phacoemulsification simulation in ophthalmology training programs. J Cataract Refract Surg 39:1616–1617. https://doi.org/10.1016/j.jcrs.2013.08.015
Rossi JV, Verma D, Fujii GY, Lakhanpal RR, Wu SL, Humayun MS, De Juan E Jr (2004) Virtual vitreoretinal surgical simulator as a training tool. Retina 24:231–236
Selvander M, Asman P (2013) Cataract surgeons outperform medical students in Eyesi virtual reality cataract surgery: evidence for construct validity. Acta Ophthalmol 91:469–474. https://doi.org/10.1111/j.1755-3768.2012.02440.x
Solverson DJ, Mazzoli RA, Raymond WR, Nelson ML, Hansen EA, Torres MF, Bhandari A et al (2009) Virtual reality simulation in acquiring and differentiating basic ophthalmic microsurgical skills. Simul Healthc 4:98–103. https://doi.org/10.1097/SIH.0b013e318195419e
Thomsen ASS, Kiilgaard JF, la Cour M, Brydges R, Konge L (2017) Is there inter-procedural transfer of skills in intraocular surgery? A randomized controlled trial. Acta Ophthalmol 95:845–851. https://doi.org/10.1111/aos.13434
Vergmann AS, Vestergaard AH, Grauslund J (2017) Virtual vitreoretinal surgery: validation of a training programme. Acta Ophthalmol 95:60–65. https://doi.org/10.1111/aos.13209
Khamis NN, Satava RM, Alnassar SA, Kern DE (2016) A stepwise model for simulation-based curriculum development for clinical skills, a modification of the six-step approach. Surg Endosc 30:279–287. https://doi.org/10.1007/s00464-015-4206-x
Thomsen AS, Kiilgaard JF, Kjaerbo H, la Cour M, Konge L (2015) Simulation-based certification for cataract surgery. Acta Ophthalmol 93:416–421. https://doi.org/10.1111/aos.12691
Thomsen AS, Bach-Holm D, Kjaerbo H, Hojgaard-Olsen K, Subhi Y, Saleh GM, Park YS et al (2017) Operating room performance improves after proficiency-based virtual reality cataract surgery training. Ophthalmology 124:524–531. https://doi.org/10.1016/j.ophtha.2016.11.015
Thomsen AS, Smith P, Subhi Y, Cour M, Tang L, Saleh GM, Konge L (2017) High correlation between performance on a virtual-reality simulator and real-life cataract surgery. Acta Ophthalmol 95:307–311. https://doi.org/10.1111/aos.13275
Smith P, Tang L, Balntas V, Young K, Athanasiadis Y, Sullivan P, Hussain B et al (2013) “PhacoTracking”: an evolving paradigm in ophthalmic surgical training. JAMA Ophthalmol 131:659–661. https://doi.org/10.1001/jamaophthalmol.2013.28
Konge L, Arendrup H, von BC, Ringsted C (2011) Using performance in multiple simulated scenarios to assess bronchoscopy skills. Respiration 81:483–490. https://doi.org/10.1159/000324452
Spiteri AV, Aggarwal R, Kersey TL, Sira M, Benjamin L, Darzi AW, Bloom PA (2014) Development of a virtual reality training curriculum for phacoemulsification surgery. Eye (Lond) 28:78–84. https://doi.org/10.1038/eye.2013.211
Cook DA, Brydges R, Zendejas B, Hamstra SJ, Hatala R (2013) Mastery learning for health professionals using technology-enhanced simulation: a systematic review and meta-analysis. Acad Med 88:1178–1186. https://doi.org/10.1097/ACM.0b013e31829a365d
Saleh GM, Gauba V, Mitra A, Litwin AS, Chung AK, Benjamin L (2007) Objective structured assessment of cataract surgical skill. Arch Ophthalmol 125:363–366. https://doi.org/10.1001/archopht.125.3.363
Feudner EM, Engel C, Neuhann IM, Petermeier K, Bartz-Schmidt KU, Szurman P (2009) Virtual reality training improves wet-lab performance of capsulorhexis: results of a randomized, controlled study. Graefes Arch Clin Exp Ophthalmol 247:955–963. https://doi.org/10.1007/s00417-008-1029-7
McCannel CA, Reed DC, Goldman DR (2013) Ophthalmic surgery simulator training improves resident performance of capsulorhexis in the operating room. Ophthalmology 120:2456–2461. https://doi.org/10.1016/j.ophtha.2013.05.003
McCannel CA (2017) Continuous curvilinear capsulorhexis training and non-rhexis related vitreous loss: the specificity of virtual reality simulator surgical training (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc 115:T2
Funding
The study was founded by Fight for Sight Denmark, velux foundation, and the Synoptik Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in these studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
la Cour, M., Thomsen, A.S.S., Alberti, M. et al. Simulators in the training of surgeons: is it worth the investment in money and time? 2018 Jules Gonin lecture of the Retina Research Foundation. Graefes Arch Clin Exp Ophthalmol 257, 877–881 (2019). https://doi.org/10.1007/s00417-019-04244-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04244-y