Abstract
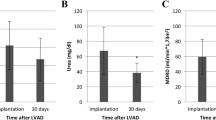
Renal replacement therapy (RRT) after continuous flow left ventricular assist device (CF-LVAD) implantation significantly affects patients’ quality of life and survival. To identify preoperative prognostic markers in patients requiring RRT after CF-LVAD implantation, we retrospectively reviewed data from patients who underwent implantation of a CF-LVAD at our institution during 2012–2017. Patients who required preoperative RRT were excluded. Preoperative and operative characteristics, as well as survival and adverse events, were compared between 74 (22.2%) patients requiring any duration of postoperative RRT and 259 (77.8%) not requiring RRT. Patients requiring RRT experienced more postoperative complications than patients who did not, including respiratory failure necessitating tracheostomy (35.7% vs 2.5%, p < 0.001), reoperation for bleeding (34.3% vs 11.7%, p < 0.001), and right heart failure necessitating perioperative mechanical circulatory support (32.4% vs 6.9%, p < 0.001). Patients requiring postoperative RRT also had poorer survival at 30 days (74.7% vs 98.8%), 6 months (48.2% vs 95.1%), and 12 months (45.3% vs 90.2%) (p < 0.001). Significant predictors of RRT after CF-LVAD implantation included urine proteinuria (odds ratio [OR] 3.6, 95% confidence interval [CI] [1.7–7.6], p = 0.001), estimated glomerular filtration rate < 45 mL/min/1.73 m2 (OR 3.4, 95% CI [1.5–17.8], p = 0.004), and mean right atrial pressure to pulmonary capillary wedge pressure ratio ≥ 0.54 (OR 2.6, 95% CI [1.3–5.], p = 0.01). Of the 74 RRT patients, 11 (14.9%) recovered renal function before discharge, 36 (48.6%) still required RRT after discharge, and 27 (36.5%) died before discharge. We conclude that preoperative renal and right ventricular dysfunction significantly predict postoperative renal failure and mortality after CF-LVAD implantation.


Similar content being viewed by others
References
Rose EA, Gelijns AC, Moskowitz AJ, Heitjan DF, Stevenson LW, Dembitsky W, et al. Long-term use of a left ventricular assist device for end-stage heart failure. N Engl J Med. 2001;345:1435–43.
Anjum A, Kurihara C, Critsinelis A, Kawabori M, Sugiura T, Civitello AB, et al. Acute kidney injury after implantation of a left ventricular assist device: a comparison of axial-flow (HeartMate II) and centrifugal-flow (HeartWare HVAD) devices. J Artif Organs. 2018;21:285–92.
Hasin T, Topilsky Y, Schirger JA, Li Z, Zhao Y, Boilson BA, et al. Changes in renal function after implantation of continuous-flow left ventricular assist devices. J Am CollCardiol. 2012;59:26–36.
Hasin T, Grupper A, Dillon JJ, Maleszewski JJ, Li Z, Topilsky Y, et al. Early gains in renal function following implantation of HeartMate II left ventricular assist devices may not persist to one year. ASAIO J. 2017;63:401–7.
Bansal N, Hailpern SM, Katz R, Hall YN, Kurella Tamura M, Kreuter W, et al. Outcomes associated with left ventricular assist devices among recipients with and without end-stage renal disease. JAMA Intern Med. 2018;178:204–9.
Feldman D, Pamboukian SV, Teuteberg JJ, Birks E, Lietz K, Moore SA, et al. The 2013 International Society for Heart and Lung Transplantation Guidelines for mechanical circulatory support: executive summary. J Heart Lung Transplant. 2013;32:157–87.
Hsu CY, Chertow GM, McCulloch CE, Fan D, Ordonez JD, Go AS. Nonrecovery of kidney function and death after acute on chronic renal failure. Clin J Am SocNephrol. 2009;4:891–8.
Kidney Disease Improving Global Outcome. KDIGO Clinical Practice Guideline for Acute Kidney Injury. 2012. https://kdigo.org/wp-content/uploads/2016/10/KDIGO-2012-AKI-Guideline-English.pdf. Accessed 17 Mar 2020.
Kidney Disease Improving Global Outcome. KDIGO Clinical Practice Guideline for Acute Kidney Injury: Online Appendices A-F. 2012. https://kdigo.org/wp-content/uploads/2016/10/KDIGO-AKI-Suppl-Appendices-A-F_March2012.pdf. Accessed 17 Mar 2020.
Soliman OII, Akin S, Muslem R, Boersma E, Manintveld OC, Krabatsch T, et al. Derivation and validation of a novel right-sided heart failure model after implantation of continuous flow left ventricular assist devices: The EUROMACS (European Registry for Patients with Mechanical Circulatory Support) right-sided heart failure risk score. Circulation. 2018;137:891–906.
Thongprayoon C, Lertjitbanjong P, Cheungpasitporn W, Hansrivijit P, Fulop T, Kovvuru K, et al. Incidence and impact of acute kidney injury on patients with implantable left ventricular assist devices: a meta-analysis. Ren Fail. 2020;42:495–512.
Silver SA, Long J, Zheng Y, Goldstone AB, Franz D, Chang TI, et al. Outcomes after left ventricular assist device implantation in patients with acute kidney injury. J ThoracCardiovascSurg. 2020;159(477–86):e3.
Genovese EA, Dew MA, Teuteberg JJ, Simon MA, Bhama JK, Bermudez CA, et al. Early adverse events as predictors of 1-year mortality during mechanical circulatory support. J Heart Lung Transplant. 2010;29:981–8.
Ross DW, Stevens GR, Wanchoo R, Majure DT, Jauhar S, Fernandez HA, et al. Left ventricular assist devices and the kidney. Clin J Am SocNephrol. 2018;13:348–55.
Sandner SE, Zimpfer D, Zrunek P, Rajek A, Schima H, Dunkler D, et al. Renal function and outcome after continuous flow left ventricular assist device implantation. Ann ThoracSurg. 2009;87:1072–8.
Walther CP, Winkelmayer WC, Niu J, Cheema FH, Nair AP, Morgan JA, et al. Acute kidney injury with ventricular assist device placement: national estimates of trends and outcomes. Am J Kidney Dis. 2019;74:650–8.
Topkara VK, Coromilas EJ, Garan AR, Li RC, Castagna F, Jennings DL, et al. Preoperative proteinuria and reduced glomerular filtration rate predicts renal replacement therapy in patients supported with continuous-flow left ventricular assist devices. Circ Heart Fail. 2016;9:e002897.
Asleh R, Schettle S, Briasoulis A, Killian JM, Stulak JM, Pereira NL, et al. Predictors and outcomes of renal replacement therapy after left ventricular assist device implantation. Mayo ClinProc. 2019;94:1003–14.
Laribi S, Mebazaa A. Cardiohepatic syndrome: liver injury in decompensated heart failure. Curr Heart Fail Rep. 2014;11:236–40.
Poelzl G, Auer J. Cardiohepatic syndrome. Curr Heart Fail Rep. 2015;12:68–78.
Topkara VK, Colombo PC. Proteinuria in left ventricular assist device candidates: an emerging risk factor for renal failure and mortality. J Heart Lung Transplant. 2018;37:143–5.
Xu S, Liu J, Li L, Wu Z, Li J, Liu Y, et al. Cardiopulmonary bypass time is an independent risk factor for acute kidney injury in emergent thoracic aortic surgery: a retrospective cohort study. J CardiothoracSurg. 2019;14:90.
Jalal DI, Chonchol M, Targher G. Disorders of hemostasis associated with chronic kidney disease. SeminThrombHemost. 2010;36:34–40.
Dijoy L, Dean JS, Bistrick C, Sistino JJ. The history of goal-directed therapy and relevance to cardiopulmonary bypass. J Extra CorporTechnol. 2015;47:90–4.
Gist KM, Kaufman J, da Cruz EM, Friesen RH, Crumback SL, Linders M, et al. A decline in intraoperative renal near-infrared spectroscopy is associated with adverse outcomes in children following cardiac surgery. PediatrCrit Care Med. 2016;17:342–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This manuscript is based on a poster presentation with the same title at the American Society of Artificial Internal Organs on June 29th, 2019 in San Francisco, CA.
Rights and permissions
About this article
Cite this article
Parikh, U., Lamba, H., Ajmal, M. et al. Predictors of renal replacement therapy in patients with continuous flow left ventricular assist devices. J Artif Organs 24, 207–216 (2021). https://doi.org/10.1007/s10047-020-01239-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-020-01239-z