Abstract
Background
Diffuse correlation spectroscopy (DCS) noninvasively permits continuous, quantitative, bedside measurements of cerebral blood flow (CBF). To test whether optical monitoring (OM) can detect decrements in CBF producing cerebral hypoxia, we applied the OM technique continuously to probe brain-injured patients who also had invasive brain tissue oxygen (PbO2) monitors.
Methods
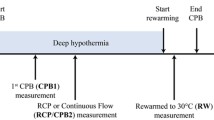
Comatose patients with a Glasgow Coma Score (GCS) < 8) were enrolled in an IRB-approved protocol after obtaining informed consent from the legally authorized representative. Patients underwent 6–8 h of daily monitoring. Brain PbO2 was measured with a Clark electrode. Absolute CBF was monitored with DCS, calibrated by perfusion measurements based on intravenous indocyanine green bolus administration. Variation of optical CBF and mean arterial pressure (MAP) from baseline was measured during periods of brain hypoxia (defined as a drop in PbO2 below 19 mmHg for more than 6 min from baseline (PbO2 > 21 mmHg). In a secondary analysis, we compared optical CBF and MAP during randomly selected 12-min periods of “normal” (> 21 mmHg) and “low” (< 19 mmHg) PbO2. Receiver operator characteristic (ROC) and logistic regression analysis were employed to assess the utility of optical CBF, MAP, and the two-variable combination, for discrimination of brain hypoxia from normal brain oxygen tension.
Results
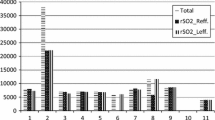
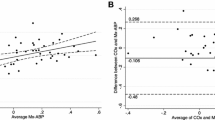
Seven patients were enrolled and monitored for a total of 17 days. Baseline-normalized MAP and CBF significantly decreased during brain hypoxia events (p < 0.05). Through use of randomly selected, temporally sparse windows of low and high PbO2, we observed that both MAP and optical CBF discriminated between periods of brain hypoxia and normal brain oxygen tension (ROC AUC 0.761, 0.762, respectively). Further, combining these variables using logistic regression analysis markedly improved the ability to distinguish low- and high-PbO2 epochs (AUC 0.876).
Conclusions
The data suggest optical techniques may be able to provide continuous individualized CBF measurement to indicate occurrence of brain hypoxia and guide brain-directed therapy.







Similar content being viewed by others
References
Anderson CS, Heeley E, Huang Y, et al. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013;368:2355–65.
Muizelaar J, Marmarou A, Ward J, et al. Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J Neurosurg. 1991;75:731–9.
Leal-Noval SR, Cayuela A, Arellano-Orden V, et al. Invasive and noninvasive assessment of cerebral oxygenation in patients with severe traumatic brain injury. Intensive Care Med. 2010;36:1309–17.
Stiefel M, Spiotta A, Gracias V, et al. Reduced mortality rate in patients with severe traumatic brain injury treated with brain tissue oxygen monitoring. J Neurosurg. 2005;103:805–11.
Rosenthal G, Hemphill JC III, Sorani M, et al. Brain tissue oxygen tension is more indicative of oxygen diffusion than oxygen delivery and metabolism in patients with traumatic brain injury. Crit Care Med. 2008;36:1917–24.
Johnston AJ, Steiner LA, Coles JP, et al. Effect of cerebral perfusion pressure augmentation on regional oxygenation and metabolism after head injury. Crit Care Med. 2005;33:189–95.
Yodh AG, Greenberg JG, Yu G, et al. Inventors; Optical Measurement of Tissue Blood Flow, Hemodynamics and Oxygenation, US Patent 8,082,015; 2011.
Durduran T, Yodh AG. Diffuse correlation spectroscopy for non-invasive, micro-vascular cerebral blood flow measurement. Neuroimage. 2014;85:51–63.
St Lawrence K, Verdecchia K, Elliott J, Diop M. Measuring cerebral hemodynamics and energy metabolism by near-infrared spectroscopy., NeuromethodsNew York: Humana Press Inc.; 2014. p. 265–92.
Boas DA, Campbell LE, Yodh AG. Scattering and imaging with diffusing temporal field correlations. Phys Rev Lett. 1995;75:1855–8.
Boas DA, Yodh AG. Spatially varying dynamical properties of turbid media probed with diffusing temporal light correlation. J Opt Soc Am A. 1997;14:192–215.
Zhou C, Eucker SA, Durduran T, et al. Diffuse optical monitoring of hemodynamic changes in piglet brain with closed head injury. J Biomed Opt. 2009;14:034015.
Buckley EM, Hance D, Pawlowski T, et al. Validation of diffuse correlation spectroscopic measurement of cerebral blood flow using phase-encoded velocity mapping magnetic resonance imaging. J Biomed Opt. 2012;17:037007.
Kim MN, Durduran T, Frangos S, et al. Noninvasive measurement of cerebral blood flow and blood oxygenation using near-infrared and diffuse correlation spectroscopies in critically brain-injured adults. Neurocrit Care. 2010;12:173–80.
Diop M, Verdecchia K, Lee TY, St Lawrence K. Calibration of diffuse correlation spectroscopy with a time-resolved near-infrared technique to yield absolute cerebral blood flow measurements. Biomed Opt Express. 2011;2:2068–82.
He L, Baker W, Kavuri V, et al. Noninvasive optical monitoring of absolute cerebral blood flow in adult human subjects (abstract). J Neurosurg Anesthesiol. 2017;29:494.
Milej D, He L, Abdalmalak A, et al. Quantification of cerebral blood flow in adults by dynamic contrast-enhanced NIRS: validation against MRI. In Biophotonics congress: biomedical optics congress 2018 (Microscopy/Translational/Brain/OTS), OSA technical digest (Optical Society of America, 2018), paper BF2C.2. 2018. https://doi.org/10.1364/BRAIN.2018.BF2C.2.
Kavuri VC, Baker W, Parthasarathy AB, Balu R, Yodh AG, Kofke A. A combined diffuse correlation and time-resolved spectroscopy instrument for continuous monitoring of absolute cerebral blood flow. Biomedical Optics 2016; 2016 2016/04/25; Fort Lauderdale, Florida: Optical Society of America. p. JW3A.8.
Dietsche G, Ninck M, Ortolf C, Li J, Jaillon F, Gisler T. Fiber-based multispeckle detection for time-resolved diffusing-wave spectroscopy: characterization and application to blood flow detection in deep tissue. Appl Opt. 2007;46:8506.
Torricelli A, Contini D, Pifferi A, et al. Time domain functional NIRS imaging for human brain mapping. Neuroimage. 2014;85:28–50.
Pifferi A, Contini D, Mora AD, Farina A, Spinelli L, Torricelli A. New frontiers in time-domain diffuse optics, a review. J Biomed Opt. 2016;21:091310.
Le Roux P, Menon DK, Citerio G, et al. Consensus summary statement of the international multidisciplinary consensus conference on multimodality monitoring in neurocritical care: a statement for healthcare professionals from the Neurocritical Care Society and the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40:1189–209.
Oddo M, Levine JM, MacKenzie L, et al. Brain hypoxia is associated with short-term outcome after severe traumatic brain injury independently of intracranial hypertension and low cerebral perfusion pressure. Neurosurgery. 2011;69:1037–45.
Spiotta AM, Stiefel MF, Gracias VH, et al. Brain tissue oxygen-directed management and outcome in patients with severe traumatic brain injury. J Neurosurg. 2010;113:571–80.
Smith M, Maggee S, Stiefel M, Bloom S, Gracias V, Le Roux P. Packed red blood cell transfusion increases local cerebral oxygenation. Crit Care Clin. 2005;33:1104–8.
Parthasarathy AB, Gannon KP, Baker WB, et al. Dynamic autoregulation of cerebral blood flow measured non-invasively with fast diffuse correlation spectroscopy. J Cereb Blood Flow Metab. 2018;38:230–40.
Czosnyka M, Smielewski P, Kirkpatrick P, Laing RJ, Menon D, Pickard JD. Continuous assessment of the cerebral vasomotor reactivity in head injury. Neurosurgery. 1997;41:11–7.
Menzel M, Soukup J, Henze D, et al. Brain tissue oxygen monitoring for assessment of autoregulation: preliminary results suggest a new hypothesis. J Neurosurg Anesthesiol. 2003;15:33–41.
Zweifel C, Castellani G, Czosnyka M, et al. Continuous assessment of cerebral autoregulation with near-infrared spectroscopy in adults after subarachnoid hemorrhage. Stroke. 2010;41:1963–8.
Selb JJ, Boas DA, Chan S-T, Evans KC, Buckley EM, Carp SA. Sensitivity of near-infrared spectroscopy and diffuse correlation spectroscopy to brain hemodynamics: simulations and experimental findings during hypercapnia. Neurophotonics. 2014;1:015005.
Watzman HM, Kurth CD, Montenegro LM, Rome J, Steven JM, Nicolson SC. Arterial and venous contributions to near-infrared cerebral oximetry. Anesthesiology. 2000;93:947–53.
Yu G, Durduran T, Zhou C, et al. Noninvasive monitoring of murine tumor blood flow during and after photodynamic therapy provides early assessment of therapeutic efficacy. Clin Cancer Res. 2005;11:3543–52.
Durduran T. Non-invasive measurements of tissue hemodynamics with hybrid diffuse optical methods. Thesis. Philadelphia: University of Pennsylvania; 2004.
Durduran T, Yu G, Burnett MG, et al. Diffuse optical measurement of blood flow, blood oxygenation, and metabolism in a human brain during sensorimotor cortex activation. Opt Lett. 2004;29:1766–8.
Cheung C, Culver JP, Takahashi K, Greenberg JH, Yodh AG. In vivo cerebrovascular measurement combining diffuse near-infrared absorption and correlation spectroscopies. Phys Med Biol. 2001;46:2053–65.
Culver JP, Durduran T, Cheung C, Furuya D, Greenberg JH, Yodh AG. Diffuse optical measurement of hemoglobin and cerebral blood flow in rat brain during hypercapnia, hypoxia and cardiac arrest. Adv Exp Med Biol. 2003;510:293–7.
Carp SA, Dai GP, Boas DA, Franceschini MA, Kim YR. Validation of diffuse correlation spectroscopy measurements of rodent cerebral blood flow with simultaneous arterial spin labeling MRI; towards MRI-optical continuous cerebral metabolic monitoring. Biomed Opt Express. 2010;1:553–65.
Baker WB, Parthasarathy AB, Ko TS, et al. Pressure modulation algorithm to separate cerebral hemodynamic signals from extracerebral artifacts. Neurophotonics. 2015;2:035004.
Funding
We acknowledge support from the National Institute of Health (R01-NS082309-01A1, R01-NS060653, P41-EB015893).
Author information
Authors and Affiliations
Contributions
DRB and WG are involved in data analysis, conceptualization of protocol, and manuscript composition contribution; RB, data analysis, patient recruitment, conceptualization of protocol, and manuscript composition contribution); WBB, data analysis, collection and organization of patient data, ICG CBF analysis, conceptualization of protocol, and manuscript composition contribution; LH, building and maintaining of instrumentation, collection and maintenance of patient data, ICG CBF analysis, and manuscript composition contribution; MD, DM, and KSL, ICG CBF analysis, manuscript composition contribution; VK, instrument construction and bioengineering; OA, data collection and management, patient enrollment, manuscript composition contribution; AGY, biomedical optics, physics and analysis oversight, conceptualization of protocol, manuscript composition contributions; WAK, conceptualization of protocol, clinical oversight, patient recruitment, and manuscript composition contribution.
Corresponding author
Ethics declarations
Conflict of interest
Several of the investigators received salary support from the National Institutes of Health, Canadian Institutes of Health Research, and the National Science Foundation; Wesley B. Baker has submitted two Patents to the US Patent office on behalf of the Trustees of the University of Pennsylvania: provisional patent number 17-8261/103241.000816, and provisional patent number 14-6924/103241.005919; Ramani Balu has participated in a patent submitted to the US Patent office on behalf of the Trustees of the University of Pennsylvania, US20160361017A1; Mamadou Diop, Olivia Amendolia, Wensheng Guo, Keith St. Lawrence, have no additional conflicts of interest to disclose; Venkaiah Kavuri works for Masimo, a biooptics corporation and has a patent US20170049417A1 pending on behalf of the University of Texas System; W. Andrew Kofke is on the editorial board of the Journal of Neurosurgical Anesthesiology and is on the editorial board of Neurocritical Care, and he has participated in a patent submitted to the US Patent office on behalf of the Trustees of the University of Pennsylvania: provisional patent number 17-8261/103241.000816; Arjun G. Yodh has his name is on eight patents submitted on behalf of the Trustees of the University of Pennsylvania, US6304771B1, US5917190A, US6076010A, US20080292164A1, US20060063995A1, US6487428B1, US6831741B1, and provisional patent number 17-8261/103241.000816. David R. Busch has a International Patent Applications PCT/US2015/017277 and PCT/US2015/017286.
Ethical Approval
The Institutional Review Board of the University of Pennsylvania approved all aspects of the study. All procedures performed were in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants’ legally authorized representatives.
Rights and permissions
About this article
Cite this article
Busch, D.R., Balu, R., Baker, W.B. et al. Detection of Brain Hypoxia Based on Noninvasive Optical Monitoring of Cerebral Blood Flow with Diffuse Correlation Spectroscopy. Neurocrit Care 30, 72–80 (2019). https://doi.org/10.1007/s12028-018-0573-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0573-1