Abstract
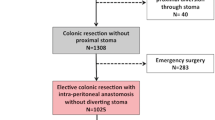
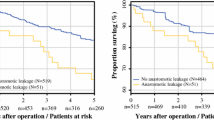
Anastomotic leakage (AL) is a serious complication of colorectal surgery as it greatly increases morbidity and mortality and has been associated with augmented local recurrence and diminished survival. Many risk factors have been identified to date, but sizable studies on AL after colorectal resection are lacking. This study aimed to identify the risk factors and postoperative complications of AL after colorectal surgery in the first affiliated hospital of Sun Yat-sen University. One thousand two hundred seventy-five patients who underwent colorectal cancer surgery between January 2010 and June 2013 were retrospectively studied. Twelve preoperative, 17 operative, and 11 postoperative variables were examined by the chi-square test or Fisher’s exact test for univariate analysis and were then further examined by multivariate logistic regression analysis, among which one operative and three postoperative variables were examined in 426 rectal cancer surgeries. Additionally, eight postoperative complications and short-term prognostic variables were also examined by the chi-square test or a Fisher’s exact test. AL was identified in 60/1158 (5.2%) total patients, 20/732 (2.7%), and 40/426 (9.4%) of whom had colonic and rectal cancer, respectively. Univariate analysis identified preoperative variables: sex (p = 0.012), preoperative carcinoembryonic antigen (CEA) level (p < 0.001), and hemoglobin level (p = 0.089); operative variables: surgical time (p = 0.009), anastomotic methods (p = 0.003), surgical staging (p = 0.016), and operative sites (p < 0.001); and postoperative pathologic variables: distance from tumor to distal incisional margin (p < 0.001). For rectal cancer, the variables included rectal procedures (p = 0.022), rectal segments (p = 0.010), distance from the tumor to the dentate line (p = 0.011) and total mesorectal excision (TME) (p = 0.046). All of these variables were included in the multivariate analysis, which identified the surgical time (p = 0.021), preoperative CEA level ≥ 41 μg/L (p < 0.001), and double-stapled anastomosis (p = 0.007); for rectal cancer, the middle or lower rectal segment (p = 0.008, 0.005, respectively) was included as an independent predictive factor for AL. Of the eight postoperative complications or short-term prognostic variables, postoperative hospital stay, abdominal infection, urologic infection, and incisional infection were considered significant. The rate of AL after rectal cancer is much higher than that of colon cancer. Surgical time, tumor biomarkers, anastomotic methods, and rectal segments may have the potential to increase the occurrence of AL. Additionally, AL may increase patients’ hospital costs, length of stay and other relevant complications.
Similar content being viewed by others
References
Kube R, Mroczkowski P, Granowski D, Benedix F, Sahm M, Schmidt U, Gastinger I, Lippert H (2010) Anastomotic leakage after colon cancer surgery: a predictor of significant morbidity and hospital mortality, and diminished tumour-free survival. Eur J Surg Oncol 36(2):120–124
Krarup PM, Jorgensen LN, Andreasen AH, Harling H, Danish Colorectal Cancer Group (2012) Danish Colorectal Cancer Group: a nationwide study on anastomotic leakage after colonic cancer surgery. Color Dis 14(10):e661–e667
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM, MRC CLASICC trial group (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365(9472):1718–1726
Milsom JW, de Oliveira O Jr, Trencheva KI, Pandey S, Lee SW, Sonoda T (2009) Long-term outcomes of patients undergoing curative laparoscopic surgery for mid and low rectal cancer. Dis Colon Rectum 52(7):1215–1222
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P (2011) Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg 253(5):890–899
Burton TP, Mittal A, Soop M (2013) Nonsteroidal anti-inflammatory drugs and anastomotic dehiscence in bowel surgery: systematic review and meta-analysis of randomized, controlled trials. Dis Colon Rectum 56(1):126–134
Morris EJ, Taylor EF, Thomas JD, Quirke P, Finan PJ, Coleman MP, Rachet B, Forman D (2011) Thirty-day postoperative mortality after colorectal cancer surgery in England. Gut 60(6):806–813
Targarona EM, Balague C, Pernas JC, Martinez C, Berindoague R, Gich I, Trias M (2008) Can we predict immediate outcome after laparoscopic rectal surgery? Multivariate analysis of clinical, anatomic, and pathologic features after 3-dimensional reconstruction of the pelvic anatomy. Ann Surg 247(4):642–649
Yang L, Huang XE, Zhou JN (2013) Risk assessment on anastomotic leakage after rectal cancer surgery: an analysis of 753 patients. Asian Pac J Cancer Prev 14(7):4447–4453
Schouten SB, De Bruin AF, Gosselink MP, Nigg AL, van Iterson M, Biermann K, Kliffen M, van der Harst E (2014) Is microvessel density correlated with anastomotic leakage after low anterior resection? Hepato-Gastroenterology 61(129):90–93
Sun LC, Chu KS, Cheng SC, Lu CY, Kuo CH, Hsieh JS, Shih YL, Chang SJ, Wang JY (2009) Preoperative serum carcinoembryonic antigen, albumin and age are supplementary to UICC staging systems in predicting survival for colorectal cancer patients undergoing surgical treatment. BMC Cancer 9:288
Gara S, Meziou S, Mtar A, Ghanem A, Harzallah L, Rahal K, Boussen H, Guemira F (2012) Prognostic value of preoperative carcinoembryonic antigen level in colorectal cancer in Tunisia. Tunis Med 90(1):41–44
Ikeda T, Kumashiro R, Taketani K, Ando K, Kimura Y, Saeki H, Oki E, Morita M, Akahoshi T, Hashizume M, Maehara Y (2015) Endoscopic evaluation of clinical colorectal anastomotic leakage. J Surg Res 193(1):126–134
Choy PY, Bissett IP, Docherty JG, Parry BR, Merrie A, Fitzgerald A (2011) Stapled versus handsewn methods for ileocolic anastomoses. Cochrane Database Syst Rev (9):CD004320. https://doi.org/10.1002/14651858.CD004320.pub3
Kim HJ, Choi GS, Park JS, Park SY (2013) Comparison of intracorporeal single-stapled and double-stapled anastomosis in laparoscopic low anterior resection for rectal cancer: a case-control study. Int J Color Dis 28(1):149–156
Eriksen MT, Wibe A, Norstein J, Haffner J, Wiig JN, Norwegian Rectal Cancer Group (2005) Anastomotic leakage following routine mesorectal excision for rectal cancer in a national cohort of patients. Color Dis 7(1):51–57
Saha AK, Chowdhury F, Jha AK, Chatterjee S, Das A, Banu P (2014) Mechanical bowel preparation versus no preparation before colorectal surgery: a randomized prospective trial in a tertiary care institute. J Nat Sci Biol Med 5(2):421–424
Yang L, Huang XE, Xu L, Zhou X, Zhou JN, Yu DS, Li DZ, Guan X (2013) Acidic pelvic drainage as a predictive factor for anastomotic leakage after surgery for patients with rectal cancer. Asian Pac J Cancer Prev 14(9):5441–5447
Peeters KC, Tollenaar RA, Marijnen CA, Klein Kranenbarg E, Steup WH, Wiggers T, Rutten HJ, van de Velde CJ, Dutch ColorectalCancer Group (2005) Risk factors for anastomotic failure after total mesorectal excision of rectal cancer. Br J Surg 92(2):211–216
Valentijn TM, Galal W, Tjeertes EK, Hoeks SE, Verhagen HJ, Stolker RJ (2013) The obesity paradox in the surgical population. Surgeon 11(3):169–176
Iancu C, Mocan LC, Todea-Iancu D, Mocan T, Acalovschi I, Ionescu D, Zaharie FV, Osian G, Puia CI, Muntean V (2008) Host-related predictive factors for anastomotic leakage following large bowel resections for colorectal cancer. J Gastrointestin Liver Dis 17(3):299–303
Law WL, Choi HK, Lee YM, Ho JW, Seto CL (2007) Anastomotic leakage is associated with poor long-term outcome in patients after curative colorectal resection for malignancy. J Gastrointest Surg 11(1):8–15
Choi HK, Law WL, Ho JW (2006) Leakage after resection and intraperitoneal anastomosis for colorectal malignancy: analysis of risk factors. Dis Colon Rectum 49(11):1719–1725
Halabi WJ, Kang CY, Nguyen VQ, Carmichael JC, Mills S, Stamos MJ, Pigazzi A (2014) Epidural analgesia in laparoscopic colorectal surgery: a nationwide analysis of use and outcomes. JAMA Surg 149(2):130–136
Lipska MA, Bissett IP, Parry BR, Merrie AE (2006) Anastomotic leakage after lower gastrointestinal anastomosis: men are at a higher risk. ANZ J Surg 76(7):579–585
Tang R, Chen HH, Wang YL, Changchien CR, Chen JS, Hsu KC, Chiang JM, Wang JY (2001) Risk factors for surgical site infection after elective resection of the colon and rectum: a single center prospective study of 2,809 consecutive patients. Ann Surg 234(2):181–189
Shrikhande SV, Gaikwad V, Desouza A, Goel M (2014) Is laparoscopic surgery the standard of care for GI luminal Cancer? Indian J Surg 76(6):444–452
Bertelsen CA, Andreasen AH, Jorgensen T, Harling H, Danish Colorectal Cancer Group (2010) Anastomotic leakage after anterior resection for rectal cancer: risk factors. Color Dis 12(1):37–43
Smith JD, Butte JM, Weiser MR, D’Angelica MI, Paty PB, Temple LK, Guillem JG, Jarnagin WR, Nash GM (2013) Anastomotic leak following low anterior resection in stage IV rectal cancer is associated with poor survival. Ann Surg Oncol 20(8):2641–2646
Mrak K, Eberl T, Laske A, Jagoditsch M, Fritz J, Tschmelitsch J (2013) Impact of postoperative complications on long-term survival after resection for rectal cancer. Dis Colon Rectum 56(1):20–28
Funding
This paper presents independent research funded by the Guangdong Natural Science Foundation (project number: 2010B080701106). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have conflicts of interest.
Rights and permissions
About this article
Cite this article
Yi, X., Huang, Y., He, Y. et al. Risk Factors Associated with Anastomotic Leakage in Colorectal Cancer. Indian J Surg 81, 154–163 (2019). https://doi.org/10.1007/s12262-018-1757-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-018-1757-9