Abstract
Objectives
To compare the values obtained from maximum respiratory pressures (MRP) between sarcopenic and non-sarcopenic elderly; to verify the association of maximum respiratory pressures with sarcopenia and its indicators; and to establish cut-off points for MRP as a discriminator of sarcopenia.
Design
Cross-sectional study.
Location
Macapá, Brazil.
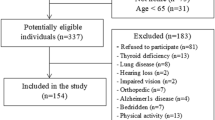
Participants
Community-dwelling elderly ≥ 60 years old, both sexes.
Measures
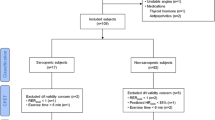
Evaluation of respiratory muscle strength (maximal inspiratory pressure - MIP and maximal expiratory pressure - MEP) and sarcopenia, according to the European Working Group on Sarcopenia in Older People (EWGSOP), in which the diagnosis of this condition considered the reduction of muscle mass (muscle mass index - MMI) associated with muscle strength reduction (hand grip strength - HGS) and / or impairment in physical performance (gait speed - GS).
Results
The sample consisted of 383 elderly individuals, with a mean age of 70.02 ± 7.3 years and a prevalence of sarcopenia of 12.53% (n = 48). Sarcopenic individuals presented significantly lower (obtained, obtained versus predicted) mean values for the maximal respiratory pressures compared to the non-sarcopenic elderly, and these were inversely associated with sarcopenia (an increase by 1 cmH2O in MIP and MEP reduced by 5% and 3%, respectively, the probability of sarcopenia). In relation to the association with the sarcopenia indicators, the increase by 1 cmH2O in MIP and MEP decreased, respectively, the probability of decreasing muscle strength (3% and 2%), GS (3% and 4%) and MMI (3 % - MIP). Cut-off points ≤60 cmH2O and ≤50 cmH2O for MEP and ≤55 cmH2O and ≤45 cmH2O for MEP, respectively for elderly men and women, served as a discriminant criterion for the presence of sarcopenia (area under the ROC curve superior to 0.70).
Conclusions
Elderly patients with sarcopenia had lower MIP and MEP values when compared to non-sarcopenic individuals, and respiratory muscle strength was inversely associated with the diagnosis of sarcopenia and its indicators (HGS, gait speed and MMI). Furthermore, cut-off points for MIP and MEP can be used in clinical practice as discriminators of sarcopenia in community-dwelling elderly.






Similar content being viewed by others
References
Reis CS, Noronha K, Wajnman S. Population aging and hospitalization expenses of SUS: an analysis performed for Brazil between 2000 and 2010. Rev. bras. estud. Popul. 2016;33(3):591–612. doi: 10.20947/s0102-30982016c0007.
Moraes EM. Atenção à saúde do idoso: aspectos conceituais. Brasil, 2012.
United Nations Organization. World population prospects: the 2017 revision, key findings and advance tables. Available: https://doi.org/esa.un.org/unpd/wpp/. Accessed 02 december 2017.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. European Working Group on Sarcopenia in Older People. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010; 39:412–23. doi: 10.1093/ageing/afq034.
Silva TAA, Frisoli Junior A, Pinheiro MM, Szejnfeld VL. Sarcopenia and aging: etiological aspects and therapeutic options. Rev. Bras. Reumatol. 2006; 46(6):391–397. doi: 10.1590/S0482-50042006000600006.
Lalley PM. The aging respiratory system-Pulmonary structure, function and neural control. Respir Physiol Neurobiol. 2013. 187(3):199–210. doi: 10.1016/j. resp.2013.03.012.
Izawa KP, Watanabe S, Oka K et al. Respiratory muscle strength in relation to sarcopenia in elderly cardiac patients. Aging Clin Exp Res. 2016;28(6):1143–1148. doi: 10.1007/s40520-016-0534-5.
Instituto Brasileiro de Geografia e Estatística, 2010. Cidades. Macapá. Available: https://doi.org/www.cidades.ibge.gov.br. Accessed 13 december 2017.
Instituto Brasileiro de Geografia e Estatística, 2010. Síntese de Indicadores Sociais: uma análise das condições de vida da população brasileira. Brasil.
Bertolucci PF, Brucki SMD, Campassi SR, Juliano IO. The Mini-Mental State Examination in an outpatient population: influence of literacy. Arq Neuropsiquiatr. 1994;52(1):1–7. doi: 10.1590/S0004-282X1994000100001.
Souza RB. Pressões respiratórias estáticas máximas. J Pneumol. 2002; 28(Supl 3):S155–65.
Fiore Jr JF, Paisani DM, Franceschini J et al. Maximal respiratory pressures and vital capacity: comparison between mouthpiece and face-mask evaluation methods. J Bras Pneumol. 2004; 30: 515–520. doi: 10.1590/S1806-37132004000600005.
Green M, Road J, Sieck GC, Similowski T. Tests of respiratory muscle strenght. Am J Respir Crit Care Med. 2002; 166:528–47.
Rubinstein I, Slutsky AS, Rebuk AS, McClean PA, Boucher R, Szeinberg A. Assessment of maximal expiratory pressure in healthy adults. J Appl Physiol. 1988;64(5):2215–19. doi: 10.1152/jappl.1988.64.5.2215.
Lee RC, Wang Z, Heo M et al. Total-body skeletal muscle mass: development and cross-validation of anthropometric prediction models. Am J Clin Nutr 2000;72:796–803.
Rech CR, Dellagrana RA, Marucci MFN et al. Validity of anthropometric equations for the estimation of muscle mass in the elderly. Rev Bras Cineantropom Desempenho Hum 2012; 14:23–31. doi: 10.5007/1980-0037.2012v14n1p23.
Alexandre TS, Duarte YA, Santos JL, Wong R, Lebrão ML. Prevalence and associated factors of sarcopenia among elderly in Brazil: findings from the SABE study. J Nutr Health Aging. 2014 Mar;18(3):284–90. doi: 10.1007/s12603-013-0413-0.
Pinheiro PA, Carneiro JA, Coqueiro RS, Pereira R, Fernandes MH. «Chair Stand Test» as Simple Tool for Sarcopenia Screening in Elderly Women. J Nutr Health Aging. 2016 Jan;20(1):56–9. doi: 10.1007/s12603-015-0621-x.
Delmonico MJ, Harris TB, Lee JS, Visser M, Nevitt M, Kritchevsky SB et al. Alternative definitions of sarcopenia, lower extremity performance, and functional impairment with aging in older men and women. J Am Geriatr Soc. 2007;55:769–774. doi: 10.1111/j.1532-5415.2007.01140.x
Newman AB, Kupelian V, Visser M et al. Sarcopenia: Alternative definitions and associations with lower extremity function. J Am Geriatr Soc. 2003;51(11):1602–9.
American Society of Hand Therapists. Clinical assessment recommendations. Chicago; 1992.
Laurentani F, Russo RC, Bandinelli S, Bartali B, Cavazzini C, Di Iorio A et al. Ageassociated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. J Appl Physiol. 2003;95(5):1851–60. doi: 10.1152/japplphysiol.00246.2003
Nakano MM (2007) Versão Brasileira da Short Physical Performance Battery -SPPB: Adaptação Cultural e Estudo da Confiabilidade. University State of Campinas.
Guralnik JM, Simonsick EM, Ferrucci L et al. Lower-Extremity function in persons over the age of 70 years as predictor of subsequent disability. N Engl J Med. 1995;332(9):556–61. doi: 10.1056/NEJM199503023320902.
Ramos LR, Perracini M, Rosa TE, Kalache A. Significance and management of disability among urban elderly residents in Brazil. J Cross Cult Gerontol. 1993;8(4):313–23. doi: 10.1007/BF00972560.
Benedetti TRB, Mazo GZ, Barros MVG. Application of the International Physical Activity Questionnaire (IPAQ) for evaluation of elderly women: concurrent validity and test-retest reprodutibility. Rev. bras. ciênc. mov. 2004;12(1):25–33.
Vaz Fragoso CA, Gill TM. Respiratory Impairment and the Aging Lung: A Novel Paradigm for Assessing Pulmonary Function. J Gerontol A Biol Sci Med Sci. 2012;67(3):264–275. doi: 10.1093/gerona/glr198.
Lowery EM, Brubaker AL, Kuhlmann E, Kovacs EJ. The aging lung. Clin Interv Aging. 2013;8:1489–1496. doi: 10.2147/CIA.S51152.
Greising SM, Mantilla CB, Gorman BA, Ermilov LG, Sieck GC. Diaphragm muscle sarcopenia in aging mice. Experimental Gerontology. 2013; 48(9):881–887. doi: 10.1016/j.exger.2013.06.001.
Greising SM, Medina-Martíneza JS, Vasdeva AK, Siecka GC, Mantillaa CB. Analysis of muscle fiber clustering in the diaphragm muscle of sarcopenic mice. Muscle Nerve. 2015;52(1):76–82. doi: 10.1002/mus.24641.
Caruso P, Albuquerque ALP, Santana PV et al. Diagnostic methods to assess inspiratory and expiratory muscle strength. J Bras Pneumol. 2015;41(2):110–123. doi: 10.1590/S1806-37132015000004474.
Souza DK, Peixoto SV. Descriptive study on the evolution of hospitalization costs for ambulatory care sensitive conditions in Brazil, 2000–2013. Epidemiol. Serv. Saúde. 2017;26(2):285–294. doi: 10.5123/s1679-49742017000200006.
Shin HI, Kim DK, Seo KM, Kang SH, Lee, SY, Son, S. Relation Between Respiratory Muscle Strength and Skeletal Muscle Mass and Hand Grip Strength in the Healthy Elderly. Ann Rehabil Med 2017;41(4):686–692. doi: 10.5535/arm.2017.41.4.686.
Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Respir J 2009;33:1165–1185. doi: 10.1183/09031936.00128008.
Scarlata S, Cesari M, Antonelli Incalzi R. Sarcopenia in COPD. Thorax. 2015;70:693–694. doi: 10.1136/thoraxjnl-2015-206929.
Elliott JE, Greising SM, Mantillaa CB, Sieck GC. Functional impact of sarcopenia in respiratory muscles. Respir Physiol Neurobiol. 2016;226:137–46. doi: 10.1016/j.resp.2015.10.001.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ohara, D.G., Pegorari, M.S., Oliveira dos Santos, N.L. et al. Respiratory Muscle Strength as a Discriminator of Sarcopenia in Community-Dwelling Elderly: A Cross-Sectional Study. J Nutr Health Aging 22, 952–958 (2018). https://doi.org/10.1007/s12603-018-1079-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-018-1079-4