Abstract
Data about incidence of invasive aspergillosis in intensive care units (ICU) are scarce and variable. Incidences ranging from 2 to 24% have been reported, which might reflect different autopsy policies amongst centres. Recent studies have shown that many patients with invasive aspergillosis do not have a haematological diagnosis. Instead, conditions such as chronic obstructive pulmonary disease and liver failure became recognized as important risk factors. The diagnosis remains difficult in these patients, since diagnostic tests have not been widely validated outside the haematological boundaries. Mechanical ventilation precludes the interpretation of clinical signs and radiological diagnosis is clouded by underlying lung pathology. Respiratory cultures lack sensitivity and specificity. At the moment, diagnosis is best made by testing for galactomannan in bronchoalveolar fluid samples (sensitivity and specificity of > 87%). Testing galactomannan in sera has limited sensitivity for the non-neutropenic. Modern diagnostic tests such as PCR and beta-glucan have never been validated in an ICU population. Due mostly to major delays in the diagnosis, mortality exceeds 50%. Although our therapeutic armamentarium against invasive aspergillosis has improved in recent years, data concerning safety and efficacy of new antifungal agents in the ICU setting are lacking.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Is Invasive Aspergillosis (IA) a Problem in the ICU?
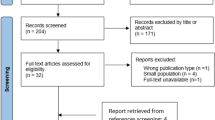
Autopsy studies show the emergence of Aspergillus as a major pathogen, as well as the expansion of the spectrum of patients at risk for IA. In a non-selected patient population, the prevalence of invasive fungal infections in an academic hospital rose from 2.2 to 5.1% over a 12-year period, largely due to an increase in Aspergillus infections [1]. However, estimates about the incidence of IA in critically ill patients are sparse and variable. For various reasons, figures about the true incidence are difficult to generate. First, in case of a positive culture for Aspergillus species, discriminating between colonisation and infection remains challenging. Second, very few institutions perform post-mortem examinations routinely, while in most cases, this is the only way for proving the definite nature of the diagnosis. Third, characteristic radiological signs of IA are usually absent in the non-neutropenic ICU patient. Finally, to date, the diagnostic utility of recently available non-culture based microbiological tools, including the detection of fungal antigens and the detection of Aspergillus-specific DNA through polymerase chain reaction (PCR) techniques, has not been properly validated in the non-haematology ICU population. In addition, typical ICU patients such as those with chronic obstructive pulmonary disease (COPD) or liver disorders were not considered amongst hosts at high risk for IA in the recently updated EORTC/MSG guidelines [2].
A summary of available studies in ICU patients is listed in Table 1 [3–9]. In a medical ICU, we have observed high incidences of IA in two separate retrospective autopsy-controlled studies. In the largest one, 127 of 1850 (6.9%) hospitalised patients had microbiological or histopathological evidence of aspergillosis during their ICU stay, including 89 cases (70%) without underlying haematological malignancy. The observed mortality of 80% was much higher than the predicted mortality as per SAPS II score (48%) [4]. An earlier study looked for unsuspected causes of death in the same medical ICU and showed that, out of 100 autopsies, there were 15 cases of IA, of which 5 were missed pre-mortem [3]. During a 6-year period, Cornillet et al. found a mean number of 15 patients per year diagnosed with IA; approximately half of them were in the ICU [9]. These inter-centre differences can be explained by differences in underlying patient characteristics, case mix and different autopsy policies.
In a recent study published by our group [10], patients with fever new lung infiltrates were screened for IA using galactomannan testing in bronchoalveolar (BAL) fluid. From a total of 1,109 patients admitted to the ICU, 110 patients fulfilled the entrance criteria and were evaluated. Most patients had non-haematological diseases (67%), including liver cirrhosis (21%), COPD (14%) and other systemic conditions (15%). The incidence of proven IA in this population was surprisingly high at 23.6%, which might have been associated with the high frequency of autopsy (95% of fatalities), as well as the use of a sensitive diagnostic tool (more comments about galactomannan testing are presented below). As this was a single-centre study, the presence of an outbreak is also a possibility.
2 Who is at Risk for Developing IA in the ICU?
Over the past two decades, IA has emerged as a life threatening fungal infection in patients with haematological diseases. Although many of these infected patients will eventually be admitted to the ICU for advanced supportive care, it seems that IA has also gained a foothold in less severely compromised ICU patients [7]. So, can a threshold of immunosuppression needed for the development of IA be defined? We grouped the risk factors for IA in the ICU are into 3 categories (high, intermediate, low) (Table 2).
Various factors adversely affect the defence systems of previously healthy individuals, including the prolonged use of antibiotics, the use of central venous catheters and/or mechanical ventilation. Although these factors are present in most ICU patients, many of them do not develop IA. One of the intriguing hypotheses for immunosuppression in the apparently immunocompetent patient with multiple organ dysfunctions is related to the biphasic response to sepsis. The initial hyperinflammatory phase is followed by relative immunoparalysis [11]. This latter process is characterized by neutrophil deactivation and may put the patient at risk for developing opportunistic infections such as IA. Further epidemiological study is warranted to better delineate this phase of immunoparalysis. More detail on the interactions between Aspergillus and the immune system are presented in the chapter by Dr Romani.
Patients in the ICU (medical and surgical) are often treated with steroids. Recent work concluded that the mortality is reduced if septic shock patients with adrenal dysfunction receive hydrocortisone for a 7-day period [12]. In vitro, however, pharmacological concentrations of hydrocortisone accelerate the growth of Aspergillus spp. [13]. Clearly, high steroid intake diminishes both lines of cellular defence against IA (macrophages and neutrophils). Palmer reported that the threshold steroid level varies according to the type of patients and emphasized that underlying lung disease is a risk factor for IA even at low doses [14]. Further study is needed to investigate whether the 7 day course of hydrocortisone at 200-mg/day in patients with septic shock puts them at risk for IA, knowing that recognition of fungal infection may be delayed, since the anti-inflammatory properties of steroids blunt the signs of infection.
Two at-risk groups not included in the EORTC/MSG definitions stand out for IA, COPD and cirrhosis patients. Patients with COPD are an increasingly recognized group of patients at risk for developing IA and in some institutions outnumber cases in “classic” patients. Bulpa et al. analyzed a group of 16 COPD patients with proven or probable IA requiring ICU admission. All patients were on steroid treatment. The outcome was invariably poor [15]. This is in accordance with the report of Rello et al., who describes another 8 COPD patients with IA and universally fatal outcome [16]. Guinea et al. from Madrid recently presented results from a large series of IA cases in association with COPD (n = 57) [17]. Steroids were identified as a risk factor in 98% of patients, with 74% of patients having received total doses of > 700 mg. Most cases of IA in COPD patients had only lung involvement, but 2 patients also had probable brain involvement. Data from the same group also revealed that COPD became the leading underlying disease associated with IA (52.4% of cases), far more frequent than classical conditions such as haematological malignancies (15.2%) [18].
Hepatic failure is generally not recognized as a risk factor for IA. A literature review revealed that 5 of 14 previously reported cases of IA in seemingly immunocompetent hosts were associated with liver disease [19]. Our study revealed 3 fatal cases of IA [4]. Patients with cirrhosis have depressed phagocytosis, which may increase their risk for severe infections.
It is expected that new risk categories of IA will come up as new immunosuppressive agents are made available such as alemtuzumab and etanercept (TNF- α blocker) [20].
3 Do Patients Acquire IA in the ICU?
There are numerous sources of Aspergillus species for patients in the ICU [21, 22]. It is believed that the primary ecological niche is decomposing material. However, aerosolised spores may become a potential source of infection through improperly cleaned ventilation systems, water systems or even computer consoles. The use of High Efficiency Particulate Air (HEPA) filtration reduces the risk of IA but does not reduce it to zero, probably partly because patients may be colonised before admission to the ICU, partly because of breaks in airflow. Pittet described two patients who developed fatal IA in the ICU. In retrospect, high concentrations of airborne Aspergillus spores could be found, closely related to air filter change in the ICU [23]. Besides the airborne route, contaminated water has been implicated as a source of infection [24]. A study of ventilators as a source of infection has not been undertaken. Of note, the development of IA is depends on an interplay between the inoculating dose, the ability of the host to resist infection (which also depends on the lung architecture) and the virulence of the infecting organism.
The concept that increasing fungal burden due to specific ICU treatments for other diseases than IA (e.g. steroids for septic shock) parallels the progression from subclinical to clinical aspergillosis, needs to be explored with more sensitive markers (e.g. PCR). PCR in respiratory secretions as a modality for surveillance is an interesting topic for research.
4 Disease Manifestations in the ICU
Generally speaking, there are types of pulmonary interactions between Aspergillus species and humans. The most frequent interaction is colonisation of the airways. This can be present in patients with defective mucociliary clearance and structural changes in the bronchial wall. These changes are present in almost every mechanically ventilated patient, making them particularly susceptible to colonisation. IA will not develop in these patients unless a critical level of immunodeficiency has been reached. The second type of interaction is allergic in nature and is beyond the scope of this review (these are discussed in other chapter in this book). The most relevant form of interaction for ICU physicians is the invasive disease that develops in persons with impaired immunity. The aggressive angioinvasive form is frequently encountered in neutropenic patients, whereas cavitating infiltrates are observed most frequently in patients on steroids, patients with COPD, cirrhosis, and solid organ transplant recipients. Other more rare presentations include endocarditis, wound infections, mediastinitis (post-cardiac surgery), infection of vascular grafts, and osteomyelitis. These are occasionally a problem in immunocompromised patients and may occur as outbreaks. Infection of the central nervous system is frequently an ominous sign and may arise from haematogenous seeding (in which the lung is the most common primary site) or spread from the sinuses or following neurosurgery.
The pathogenesis of IA in steroid-immunosuppressed patients differs greatly from that in neutropenic patients. Data demonstrate that the pathological lesions are often widespread and that death is related to a high fungal burden in neutropenic animals, while the pathogenesis in non-neutropenic, steroid-treated animals is driven by an adverse inflammatory host response, frequently confined to the lungs, with a low fungal burden in the lung parenchyma and other organs [25, 26]. The reader is referred to the chapter by Drs Ben-Ami and Kontoyiannis for more detail on the pathogenesis of IA.
Clinical signs are usually non-specific and do not necessarily differ from other causes of nosocomial pneumonia. In addition, critically ill patients with prolonged stays in the ICU often develop pulmonary infiltrates, atelectasis and/or acute respiratory distress syndrome (ARDS), whereas patients with prior lung disease (e.g. COPD) may present with pre-existing cavities on conventional chest radiographs (Fig. 1).
Chest X-ray from a COPD patient on steroids, admitted to the ICU because of an exacerbation with respiratory failure. Patchy, hazy infiltrates with predominantly a peripheral localisation and a right sided pleural effusion were seen. BAL culture was positive for Haemophilus influenzae and negative for fungi. Serum galactomannan was negative but showed a value of 2.6 ng/ml in the BAL fluid. Despite treatment with caspofungin (patient was in renal failure), he died and autopsy showed invasive aspergillosis, confined to the lungs
5 Are the Available Diagnostic Tools Applicable to Patients in the ICU?
Making a timely diagnosis of IA in the ICU population is probably even more challenging than establishing an early diagnosis in patients with haematological disease, basically because the index of suspicion is lower since most patients do not belong to one of the well-established risk groups. Moreover, the diagnostic tools were mainly developed in haematological patients. In general, the diagnosis is based on a combination of compatible clinical findings, radiological abnormalities, and microbiological confirmation or on the histological proof of tissue invasion by the fungus. Table 3 gives an overview of the available diagnostic tools.
Over the past few years, lung computed tomography (CT) scan has become one of the most important tools for the diagnosis of IA [27]. Virtually diagnostic signs for angioinvasive pulmonary mycosis – not only due to aspergillosis but occasionally also due to zygomycosis as well as other vascular conditions – include single or multiple small nodules with a “halo” sign. It should be recognized that the utility of this sign has been evaluated almost exclusively in neutropenic patients. In other groups, including ICU patients, similar CT-findings are frequently absent and, if present, are far less specific [4]. Many ICU patients have non-specific interfering radiological abnormalities due to atelectasis, or ARDS (Figs. 2, 3, and 4).
Chest X-ray from a liver transplant recipient reveals predominantly right sided air-space disease. No nodular lesions are seen. Findings are compatible with the diagnosis of pneumonia. Chest CT scan was not feasible because of high FiO2 requirements. BAL culture results were negative for bacteria and fungi (while on broad spectrum antibiotics). Galactomannan in serum was negative. Patient died and autopsy showed disseminated aspergillosis
Chest X-ray and CT scan from a patient on high dose steroids because of graft-versus-host disease 4 months after haematological stem cell transplantation for acute myeloid leukaemia. Chest X-ray reveals a right-sided pleural effusion and adjacent lung infiltrate. CT scan confirms a right sided complicated parapneumonic effusion, a mass filled partially with air between the 4th and 5th rib (with partial destruction of the bone) and a wedge-shaped infiltrate on the left side. In the culture specimen of the pleural fluid grew Aspergillus fumigatus. Findings are compatible with a bronchopleural fistula, secondary to rupture of a cavitating infiltrate and adjacent bone destruction
Chest X-ray and CT scan 2 months post kidney transplantion for end stage diabetes. Bilateral lower lobe cavities with adjacent pleural effusion on the right side are seen. Transbronchial biopsy revealed Aspergillus fumigatus. Serum and BAL galactomannan was 0.1 and 5.7 ng/ml, respectively. Despite antifungal treatment, patient died of proven Aspergillus endocarditis of the tricuspid valve
A positive respiratory specimen by culture or by direct microscopic examination is present in only half of the patients with IA. The predictive value of a positive culture depends largely on the immunocompromised status of the patient and ranges from 20 to 80%. Given the ubiquitous nature of Aspergillus spores, differentiating colonisation from infection remains problematic. Two studies have examined the significance of isolation of Aspergillus spp. in ICU patients and confirmed the poor positive predictive values [7, 28]. Therefore, surveillance cultures in the ICU will add little to the diagnosis of IA.
Serological techniques based on the detection of circulating fungal cell wall components such as galactomannan (GM) or β-D-glucan and detection of circulating fungal DNA by PCR techniques hold promise in patients with haematological malignancy but limited data exist with the use of these tests in diagnosis of IA in the ICU [10]. Although very useful in the haematological patient [29], serum GM is not a sensitive marker for IA in the non-neutropenic individual, as demonstrated in lung and liver transplant recipients [30, 31]. Viable fungi could endure in the lung tissue (with encapsulation by an inflammatory process), while circulating markers remain undetectable because of clearance by circulating neutrophils. BAL fluid could be a better specimen for GM detection as recently was demonstrated in a prospective study performed in a medical ICU in a tertiary referral hospital [10]. This is reinforced by the data with the solid organ transplant population [32–34]. On the other hand, GM testing in BAL fluid samples seems very promising for the diagnosis of IA in non-neutropenic patients [10, 35]. Results from a single ICU showed that test sensitivity and specificity were 88 and 87%, respectively using a cut-off of 0.5 for BAL testing. In contrast, the sensitivity of serum GM was 42% only. A bit of caution, however, is required with this, since the best cut-off for GM testing in BAL fluid samples is still a matter of debate. It has been demonstrated experimentally that the dynamics of IA result in higher and earlier release of GM in the alveoli, in comparison to the endothelial compartment [36]. Accordingly, many studies have shown that testing GM in BAL fluid samples result in higher optical densities than testing sera [33, 37]. In a study with non-immunocompromised patients, all cases of IA were associated with GM optical densities of ≥ 1.18 in the BAL [34]. A higher cut-off value for BAL has also been suggested by other authors, in comparison to sera [32, 33]. False-positive results have been observed when BAL is tested for GM in patients colonised with Aspergillus species, particularly lung transplant recipients [32] (Dr. Pasqualotto, unpublished data).
Although attractive, other modern diagnostic tests have not been systematically evaluated for the diagnosis of IA in ICU patients. The use of β-D-glucan detection in ICU is hampered by false-positive readings (use of albumin, wound gauze, hemodialysis and bacterial infections) [38]. Galactomannan gives less false-positive results, although the presence of β-lactam antibiotics such as piperacillin-tazobactam may pose also a problem [39]. The impact of piperacillin-tazobactam is probably reduced if GM is tested in the BAL fluid instead of sera, since the epithelial lining fluid concentration of piperacillin is about half of the serum steady state concentrations [40]. Thus far, no prospective data on PCR detection are available in ICU patients, and the usefulness of combining different diagnostic test in these patients is also unknown.
6 Antifungals for the Treatment of IA in the ICU
Treatment options for IA are reviewed in the chapter by Dr Marr. In summary, amphotericin B deoxycholate was the mainstay for the treatment of IA for a long time. However, this formulation is infamous for the occurrence of serious side effects (e.g., nephrotoxicity, hypokalemia, and infusion-related reactions). These events often result in the use of suboptimal dosing regimens. Recently voriconazole, a derivative of fluconazole, has become the new standard of care for treating IA [41]. Caspofungin, micafungin, and anidulafungin belong to a new class of antifungal drugs, the echinocandins, which act by inhibiting the synthesis of ß-(1,3)-D-glucan in the fungal cell wall. Echinocandins display activity against Aspergillus species, as demonstrated in several salvage studies, but convincing first-line data are still lacking.
However, most patients recruited in these first- and second-line treatment studies suffered from an underlying haematological disorder or were transplant recipients. Patients with baseline characteristics that are commonly seen in ICU patients have usually been excluded from these studies, including those with liver function abnormalities, coagulation disorders, or renal dysfunction, and patients in need of advanced cardiovascular or pulmonary support including mechanical ventilation. Therefore, data on antifungal treatment in the ICU remain anecdotal.
In addition, many aspects of antifungal therapy that are relevant to the ICU population have not been sufficiently addressed in clinical studies, including the pharmacokinetic profile of antifungals in patients with underlying renal, hepatic and/or cardiac dysfunction; the dose-response relationship; and the best route of administration (oral, enteral, or parenteral). For instance, a recent study showed found nasogastric/gastric administration of voriconazole to be an independent predictor for undetectable voriconazole serum concentrations [42]. Other important questions that should be better addressed include the monitoring of drug-related toxicities, and especially drug interactions with frequently used “ICU-drugs”.
7 Future Directions
In an era of increased availability of new immunosuppressive drugs and better intensive care with prolonged survival, we can expect a continuing rise in the incidence of IA. Its occurrence in ICU usually entails a poor prognosis despite major recent improvements in the diagnosis and treatment of IA in patients with haematological diseases. Multicenter studies are warranted to explore the exact incidence of IA in the ICU and to better delineate the difference between hospital-acquired, ICU-acquired and community-acquired aspergillosis. Evaluating the value of galactomannan, β-D-glucan and PCR in non-neutropenic critically ill patients in different sample types (and especially in respiratory samples) is urgently needed as well as a better delineation of the patient population at risk for IA in the broad group of critically ill patients. Finally, antifungal pharmacokinetics and pharmacodynamics and interactions with other drugs need to be explored more thoroughly. Meanwhile, all new diagnostic techniques and therapeutic measures must be validated against post-mortem findings, since only proven cases offer the most valuable information.
References
Groll, A. H., Shah, P. M., Mentzel, C., Schneider, M., Just-Nuebling, G. & Huebner, K. (1996) Trends in the postmortem epidemiology of invasive fungal infections at a university hospital. J Infect, 33, 23–32.
De Pauw, B., Walsh, T. J., Donnelly, J. P., Stevens, D. A., Edwards, J. E., Calandra, T., Pappas, P. G., Maertens, J., Lortholary, O., Kauffman, C. A., Denning, D. W., Patterson, T. F., Maschmeyer, G., Bille, J., Dismukes, W. E., Herbrecht, R., Hope, W. W., Kibbler, C. C., Kullberg, B. J., Marr, K. A., Munoz, P., Odds, F. C., Perfect, J. R., Restrepo, A., Ruhnke, M., Segal, B. H., Sobel, J. D., Sorrell, T. C., Viscoli, C., Wingard, J. R., Zaoutis, T. & Bennett, J. E. (2008) Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis, 46, 1813–21.
Roosen, J., Frans, E., Wilmer, A., Knockaert, D. C. & Bobbaers, H. (2000) Comparison of premortem clinical diagnoses in critically iII patients and subsequent autopsy findings. Mayo Clin Proc, 75, 562–7.
Meersseman, W., Vandecasteele, S. J., Wilmer, A., Verbeken, E., Peetermans, W. E. & Van Wijngaerden, E. (2004) Invasive aspergillosis in critically ill patients without malignancy. Am J Respir Crit Care Med, 170, 621–5.
Dimopoulos, G., Piagnerelli, M., Berre, J., Salmon, I. & Vincent, J. L. (2004) Post mortem examination in the intensive care unit: still useful? Intensive Care Med, 30, 2080–5.
Kumar, A., Roberts, D., Wood, K. E., Light, B., Parrillo, J. E., Sharma, S., Suppes, R., Feinstein, D., Zanotti, S., Taiberg, L., Gurka, D. & Cheang, M. (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med, 34, 1589–96.
Vandewoude, K. H., Blot, S. I., Depuydt, P., Benoit, D., Temmerman, W., Colardyn, F. & Vogelaers, D. (2006) Clinical relevance of Aspergillus isolation from respiratory tract samples in critically ill patients. Crit Care, 10, R31.
Valles, J., Mesalles, E., Mariscal, D., Del Mar Fernandez, M., Pena, R., Jimenez, J. L. & Rello, J. (2003) A 7-year study of severe hospital-acquired pneumonia requiring ICU admission. Intensive Care Med, 29, 1981–8.
Cornillet, A., Camus, C., Nimubona, S., Gandemer, V., Tattevin, P., Belleguic, C., Chevrier, S., Meunier, C., Lebert, C., Aupee, M., Caulet-Maugendre, S., Faucheux, M., Lelong, B., Leray, E., Guiguen, C. & Gangneux, J. P. (2006) Comparison of epidemiological, clinical, and biological features of invasive aspergillosis in neutropenic and nonneutropenic patients: a 6-year survey. Clin Infect Dis, 43, 577–84.
Meersseman, W., Lagrou, K., Maertens, J., Wilmer, A., Hermans, G., Vanderschueren, S., Spriet, I., Verbeken, E. & Van Wijngaerden, E. (2008) Galactomannan in bronchoalveolar lavage fluid: a tool for diagnosing aspergillosis in intensive care unit patients. Am J Respir Crit Care Med, 177, 27–34.
Hartemink, K. J., Paul, M. A., Spijkstra, J. J., Girbes, A. R. & Polderman, K. H. (2003) Immunoparalysis as a cause for invasive aspergillosis? Intensive Care Med, 29, 2068–71.
Annane, D., Sebille, V., Charpentier, C., Bollaert, P. E., Francois, B., Korach, J. M., Capellier, G., Cohen, Y., Azoulay, E., Troche, G., Chaumet-Riffaud, P. & Bellissant, E. (2002) Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA, 288, 862–71.
Lionakis, M. S. & Kontoyiannis, D. P. (2003) Glucocorticoids and invasive fungal infections. Lancet, 362, 1828–38.
Palmer, L. B., Greenberg, H. E. & Schiff, M. J. (1991) Corticosteroid treatment as a risk factor for invasive aspergillosis in patients with lung disease. Thorax, 46, 15–20.
Bulpa, P. A., Dive, A. M., Garrino, M. G., Delos, M. A., Gonzalez, M. R., Evrard, P. A., Glupczynski, Y. & Installe, E. J. (2001) Chronic obstructive pulmonary disease patients with invasive pulmonary aspergillosis: benefits of intensive care? Intensive Care Med, 27, 59–67.
Rello, J., Esandi, M. E., Mariscal, D., Gallego, M., Domingo, C. & Valles, J. (1998) Invasive pulmonary aspergillosis in patients with chronic obstructive pulmonary disease: report of eight cases and review. Clin Infect Dis, 26, 1473–5.
Guinea, J., Torres-Narbona, M., Gijón, P., Peláez, T., Muñoz, P., De Miguel, J. & Bouza, E. (2008) Invasive Pulmonary Aspergillosis (IPA) in Patients with COPD: A Description of 57 Cases Collected in a Single Tertiary Hospital (1999–2008). In 48th Interscience Conference on Antimicrobial Agents and Chemotherapy. Washington, USA.
Guinea, J., Jensen, N., Torres-Narbona, M., Gijón, P., Muñoz, P. & Bouza, E. (2008) Chronic Obstructive Pulmonary Disease (COPD) is Currently the Most Common Predisposing Condition to Invasive Aspergillosis. In 48th Interscience Conference on Antimicrobial Agents and Chemotherapy. Washington, USA.
Ascah, K. J., Hyland, R. H., Hutcheon, M. A., Urbanski, S. J., Pruzanski, W., St Louis, E. L., Jones, D. P. & Keystone, E. C. (1984) Invasive aspergillosis in a “healthy” patient. Can Med Assoc J, 131, 332–5.
Martin, S. I., Marty, F. M., Fiumara, K., Treon, S. P., Gribben, J. G. & Baden, L. R. (2006) Infectious complications associated with alemtuzumab use for lymphoproliferative disorders. Clin Infect Dis, 43, 16–24.
Carlson, G. L., Mughal, M. M., Birch, M. & Denning, D. W. (1996) Aspergillus wound infection following laparostomy. J Infect, 33, 119–21.
Pasqualotto, A. C. & Denning, D. W. (2006) Post-operative aspergillosis. Clin Microbiol Infect, 12, 1060–76.
Pittet, D., Huguenin, T., Dharan, S., Sztajzel-Boissard, J., Ducel, G., Thorens, J. B., Auckenthaler, R. & Chevrolet, J. C. (1996) Unusual cause of lethal pulmonary aspergillosis in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med, 154, 541–4.
Anaissie, E. J. & Costa, S. F. (2001) Nosocomial aspergillosis is waterborne. Clin Infect Dis, 33, 1546–8.
Balloy, V., Huerre, M., Latge, J. P. & Chignard, M. (2005) Differences in patterns of infection and inflammation for corticosteroid treatment and chemotherapy in experimental invasive pulmonary aspergillosis. Infect Immun, 73, 494–503.
Chamilos, G., Luna, M., Lewis, R. E., Bodey, G. P., Chemaly, R., Tarrand, J. J., Safdar, A., Raad, II & Kontoyiannis, D. P. (2006) Invasive fungal infections in patients with hematologic malignancies in a tertiary care cancer center: an autopsy study over a 15-year period (1989–2003). Haematologica, 91, 986–9.
Greene, R. E., Schlamm, H. T., Oestmann, J. W., Stark, P., Durand, C., Lortholary, O., Wingard, J. R., Herbrecht, R., Ribaud, P., Patterson, T. F., Troke, P. F., Denning, D. W., Bennett, J. E., De Pauw, B. E. & Rubin, R. H. (2007) Imaging findings in acute invasive pulmonary aspergillosis: clinical significance of the halo sign. Clin Infect Dis, 44, 373–9.
Garnacho-Montero, J., Amaya-Villar, R., Ortiz-Leyba, C., Leon, C., Alvarez-Lerma, F., Nolla-Salas, J., Iruretagoyena, J. R. & Barcenilla, F. (2005) Isolation of Aspergillus spp. from the respiratory tract in critically ill patients: risk factors, clinical presentation and outcome. Crit Care, 9, R191–9.
Pfeiffer, C. D., Fine, J. P. & Safdar, N. (2006) Diagnosis of invasive aspergillosis using a galactomannan assay: a meta-analysis. Clin Infect Dis, 42, 1417–27.
Husain, S., Kwak, E. J., Obman, A., Wagener, M. M., Kusne, S., Stout, J. E., Mccurry, K. R. & Singh, N. (2004) Prospective assessment of Platelia Aspergillus galactomannan antigen for the diagnosis of invasive aspergillosis in lung transplant recipients. Am J Transplant, 4, 796–802.
Kwak, E. J., Husain, S., Obman, A., Meinke, L., Stout, J., Kusne, S., Wagener, M. M. & Singh, N. (2004) Efficacy of galactomannan antigen in the Platelia Aspergillus enzyme immunoassay for diagnosis of invasive aspergillosis in liver transplant recipients. J Clin Microbiol, 42, 435–8.
Clancy, C. J., Jaber, R. A., Leather, H. L., Wingard, J. R., Staley, B., Wheat, L. J., Cline, C. L., Rand, K. H., Schain, D., Baz, M. & Nguyen, M. H. (2007) Bronchoalveolar lavage galactomannan in diagnosis of invasive pulmonary aspergillosis among solid-organ transplant recipients. J Clin Microbiol, 45, 1759–65.
Husain, S., Clancy, C. J., Nguyen, M. H., Swartzentruber, S., Leather, H., Lemonte, A. M., Durkin, M. M., Knox, K. S., Hage, C. A., Bentsen, C., Singh, N., Wingard, J. R. & Wheat, L. J. (2008) Performance characteristics of the platelia Aspergillus enzyme immunoassay for detection of Aspergillus galactomannan antigen in bronchoalveolar lavage fluid. Clin Vaccine Immunol, 15, 1760–3.
Nguyen, M. H., Jaber, R., Leather, H. L., Wingard, J. R., Staley, B., Wheat, L. J., Cline, C. L., Baz, M., Rand, K. H. & Clancy, C. J. (2007) Use of bronchoalveolar lavage to detect galactomannan for diagnosis of pulmonary aspergillosis among nonimmunocompromised hosts. J Clin Microbiol, 45, 2787–92.
Anaissie, E. J. (2008) A bad bug takes on a new role as a cause of ventilator-associated pneumonia. Am J Respir Crit Care Med, 177, 1–2.
Hope, W. W., Kruhlak, M. J., Lyman, C. A., Petraitiene, R., Petraitis, V., Francesconi, A., Kasai, M., Mickiene, D., Sein, T., Peter, J., Kelaher, A. M., Hughes, J. E., Cotton, M. P., Cotten, C. J., Bacher, J., Tripathi, S., Bermudez, L., Maugel, T. K., Zerfas, P. M., Wingard, J. R., Drusano, G. L. & Walsh, T. J. (2007) Pathogenesis of Aspergillus fumigatus and the kinetics of galactomannan in an in vitro model of early invasive pulmonary aspergillosis: implications for antifungal therapy. J Infect Dis, 195, 455–66.
Penack, O., Rempf, P., Graf, B., Blau, I. W. & Thiel, E. (2008) Aspergillus galactomannan testing in patients with long-term neutropenia: implications for clinical management. Ann Oncol, 19, 984–9.
Digby, J., Kalbfleisch, J., Glenn, A., Larsen, A., Browder, W. & Williams, D. (2003) Serum glucan levels are not specific for presence of fungal infections in intensive care unit patients. Clin Diagn Lab Immunol, 10, 882–5.
Sulahian, A., Touratier, S. & Ribaud, P. (2003) False positive test for Aspergillus antigenemia related to concomitant administration of piperacillin and tazobactam. N Engl J Med, 349, 2366–7.
Boselli, E., Breilh, D., Cannesson, M., Xuereb, F., Rimmele, T., Chassard, D., Saux, M. C. & Allaouchiche, B. (2004) Steady-state plasma and intrapulmonary concentrations of piperacillin/tazobactam 4 g/0.5 g administered to critically ill patients with severe nosocomial pneumonia. Intensive Care Med, 30, 976–9.
Herbrecht, R., Denning, D. W., Patterson, T. F., Bennett, J. E., Greene, R. E., Oestmann, J. W., Kern, W. V., Marr, K. A., Ribaud, P., Lortholary, O., Sylvester, R., Rubin, R. H., Wingard, J. R., Stark, P., Durand, C., Caillot, D., Thiel, E., Chandrasekar, P. H., Hodges, M. R., Schlamm, H. T., Troke, P. F. & De Pauw, B. (2002) Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med, 347, 408–15.
Potoski, B. A., Clarke, L. G., Venkataramanan, R. & Clancy, C. J. (2008) Clinical Risk Factors for Undetectable Voriconazole (V) Serum Concentrations voriconazole level,risk factors. In 48th Interscience Conference on Antimicrobial Agents and Chemotherapy. Washington, USA.
Caillot, D., Casasnovas, O., Bernard, A., Couaillier, J. F., Durand, C., Cuisenier, B., Solary, E., Piard, F., Petrella, T., Bonnin, A., Couillault, G., Dumas, M. & Guy, H. (1997) Improved management of invasive pulmonary aspergillosis in neutropenic patients using early thoracic computed tomographic scan and surgery. J Clin Oncol, 15, 139–47.
Perfect, J. R., Cox, G. M., Lee, J. Y., Kauffman, C. A., De Repentigny, L., Chapman, S. W., Morrison, V. A., Pappas, P., Hiemenz, J. W. & Stevens, D. A. (2001) The impact of culture isolation of Aspergillus species: a hospital-based survey of aspergillosis. Clin Infect Dis, 33, 1824–33.
Bouza, E., Guinea, J., Pelaez, T., Perez-Molina, J., Alcala, L. & Munoz, P. (2005) Workload due to Aspergillus fumigatus and significance of the organism in the microbiology laboratory of a general hospital. J Clin Microbiol, 43, 2075–9.
Tuon, F. F. (2007) A systematic literature review on the diagnosis of invasive aspergillosis using polymerase chain reaction (PCR) from bronchoalveolar lavage clinical samples. Rev Iberoam Micol, 24, 89–94.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2009 Springer Science+Business Media B.V.
About this chapter
Cite this chapter
Meersseman, W. (2009). Invasive Aspergillosis in the Intensive Care Unit: Beyond the Typical Haematological Patient. In: Comarú Pasqualotto, A. (eds) Aspergillosis: From Diagnosis to Prevention. Springer, Dordrecht. https://doi.org/10.1007/978-90-481-2408-4_29
Download citation
DOI: https://doi.org/10.1007/978-90-481-2408-4_29
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-90-481-2407-7
Online ISBN: 978-90-481-2408-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)