Learning Objectives
After reading this chapter and answering the discussion questions that follow, you should be able to
-
Explain the global burden of malaria, discuss its clinical manifestations, and appraise its health impact on women and children.
-
Analyze the mechanisms and consequences of malaria and HIV co-infection and discuss current treatment, control and prevention strategies.
-
Describe the challenges posed by vector resistance to insecticides, parasite resistance to antimalarials, climate change, wars/conflicts, and HIV/AIDS to malaria control and prevention efforts.
-
Evaluate social, cultural, and economic limitations of community-based programs for malaria control and prevention.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Human Immunodeficiency Virus
- Malaria Transmission
- Malaria Control
- Cerebral Malaria
- Uncomplicated Malaria
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Malaria is caused by Plasmodium, a protozoan parasite transmitted through the bite of infected female anopheline mosquitoes. The four species of Plasmodium known to cause malaria in humans are P. falciparum, P. malariae, P. ovale, and P. vivax. Plasmodium falciparum is the most virulent of these species and is responsible for most cases of malaria infections and malaria deaths in sub-Saharan Africa. Plasmodium vivax, the second most common species of the malaria parasite, is more prevalent in Asia and is rarely associated with acute complications of malaria or fatality. Box 12.1 presents definitions of some of the most commonly used terms in malaria epidemiology.
Burden of Malaria
Figure 12.3 illustrates the various pathways by which malaria contributes to poverty, under-development, malnutrition, and maternal and infant mortality. Some 300–500 million malaria episodes occur annually. Children under 5 years of age in sub-Saharan Africa and women who are pregnant for the first or second time bear the heaviest burden of malaria morbidity and mortality. An estimated 250 million episodes of clinical malaria occur in young sub-Saharan African children annually. About 1 million cases are cerebral malaria, 4 million cases are severe anemia, and approximately 1 million result in death. Estimates of malaria mortality show wide variation. A review of the literature on this subject shows that the number of deaths due to malaria in African children aged less than 5 years could be between 625,000 and 1,824,000 annually (Breman et al. 2004).
About 250,000 of those that survive develop sequelae from neurological complications of P. falciparum malaria. Pregnant women are more vulnerable to adverse consequences of malaria than other adults. An estimated 10 million infections occur in pregnant women annually, resulting in 500,000 cases of severe maternal anemia and 500,000 low birth weight babies (Greenwood et al. 2005). In malaria-endemic countries of Africa, up to 40% of all outpatient clinic visits and between 20 and 50% of all hospital admissions are due to malaria (WHO 2003). Although the incidence of uncomplicated malaria is lower in adolescents aged 10–19 years than younger school aged and preschool children, the burden of malaria in this age group could be substantial in areas with high and stable transmission. A recent review of the epidemiology and pattern of malaria in adolescents estimates the clinical malaria rate in African adolescents aged 10–20 years to be 0.252 attacks per adolescent per year (Lalloo et al. 2006). Results of analyses based on rainfall and temperature data and geographic information system (GIS) population databases in areas with high and stable malaria transmission put the yearly estimate of the number of malaria attacks in children aged 0–4 years, 5–9 years, and 10–14 years at 81.3 million, 16.0 million, and 13.4 million, respectively.
Clinical Manifestation of Malaria
The clinical pattern and deleterious consequences of malaria infection vary, depending on the level of acquired malaria immunity of the individual and the pattern of malaria transmission in an area. In areas with high and stable malaria transmission, resident adults and older children acquire sufficient partial immunity to reduce the risk of severe and fatal malaria but younger children and pregnant women remain vulnerable to severe and complicated malaria. Malaria infection may be asymptomatic or symptomatic. The majority of malaria infections in areas where transmission is high and stable are asymptomatic. Even when malaria infection is asymptomatic, it is believed that the high prevalence of low parasitemic and asymptomatic malaria infections contribute to the high prevalence of mild and moderate childhood anemia. In these settings, young children who are less immune to the disease are more likely to have clinical malaria following infections.
The common symptoms of uncomplicated malaria are fever, poor appetite, aches, malaise, nausea, and vomiting. Uncomplicated malaria is the most common reason for which children and adults use the health service in sub-Saharan Africa. Uncomplicated malaria accounts for about 40 and 30% of outpatient attendance and hospital admissions, respectively. Malaria is also a leading cause of absenteeism and poor performance at work and school. Uncomplicated malaria is rarely fatal when treated promptly with effective antimalarial drugs. In preschool children, delayed treatment or failure to treat uncomplicated falciparum malaria could lead to rapid disease progression to severe and potentially fatal malaria within a period often less than 48 h from onset of illness. Plasmodium falciparum causes severe malaria through complex processes that involve immunological substances known as cytokines (John et al. 2000) leading to impaired perfusion and damage to tissues and organs. These pathological changes lead to clinical and laboratory features that are characteristic of severe and complicated malaria, namely cerebral malaria that is associated with impaired consciousness, repeated convulsions, severe malarial anemia, hypoglycemia, respiratory distress, and circulatory collapse. Children that die from malaria would have one or more of these signs. The risk of death is higher in patients with multiple signs (Schellenberg et al. 1999). Case fatality rate of complicated falciparum malaria is 10–50%. About 10–17% of those that survive cerebral malaria have residual neurological problems such as dyskinesia, cortical blindness, seizures, and learning disorders (Meremikwu et al.1997). Most of these disorders are resolved within 6 months but about 2% persist for longer periods of time causing varying degrees of disability and impaired intellectual development (Murphy and Breman 2001).
Consequences of Malaria in Children and Adolescents
Anemia
Childhood anemia in low-income countries is caused by multiple factors including poor nutrition, malaria, intestinal parasites, HIV/AIDS, and inherited blood disorders (e.g., glucose-6-phosphate dehydrogenase (G-6-P-D) deficiency and sickle cell disease). In areas with high transmission, malaria is the leading etiological factor for anemia. The processes by which malaria causes anemia are not yet fully understood; however, malaria-related toxins and immunological factors are believed to cause increased hemolysis, increased splenic clearance of infected and uninfected red blood cells, and impaired production of red blood cells in the bone marrow (dyserythropoeisis). In areas of Africa with high malaria transmission, surveys have shown high prevalence rates of anemia (hemoglobin <11 g/dL) among infants and children under 5 years of age (as high as 50–80% in several areas). Most of these cases of anemia go unnoticed and untreated because they are mild and cause no symptoms. Although children with mild and chronic anemia do not feel distinct symptoms of illness, mild anemia is associated with chronic debility. It can cause such adverse effects as reduced activity and impaired cognition and learning. These chronic effects of malarial anemia in concert with malaria-related school absenteeism and neurological complications from cerebral malaria, adversely affect childhood development and education in sub-Saharan Africa (Mung’Ala-Odera et al. 2004).
Severe anemia (hemoglobin <5 g/dL) is a common acute complication of falciparum malaria. It is responsible for high case fatality and often follows massive hemolysis from a single episode of falciparum malaria. Repeated episodes or poorly treated episodes of uncomplicated malaria are fairly common pathways to severe anemia in infants and young children who are residents of areas with high and stable malaria transmission. In many communities in Africa where there are high levels of P. falciparum resistance to chloroquine and sulphadoxine–pyrimethamine, the continued use of failed drugs has resulted in an increase in the incidence of severe malarial anemia. Case fatality from severe malarial anemia varies from 1% in treated cases to over 30% when associated with other complications of falciparum malaria, especially respiratory distress and deep coma (John et al. 2000). Many more children with life-threatening severe malaria anemia do not have access to formal health care where adequate treatment and blood transfusion are possible. This indicates that overall case fatality from severe malarial anemia is likely to be much higher than reported. Blood transfusion for severe malaria-related anemia accounts for a remarkable proportion of new pediatric HIV infections in Africa (Crawley and Nahlen 2004).
Given the multifactorial nature of the etiology of childhood anemia, interventions to prevent or treat it should involve several approaches. For instance, mass de-worming of children and micronutrient supplementation programs are interventions that have the potential to reduce the burden of childhood anemia in developing countries (Briand et al. 2007). Insecticide-treated nets, chemoprophylaxis, and intermittent preventive treatment are malaria-specific interventions that have been shown to significantly reduce morbidity and mortality from malaria-related anemia (Briand et al. 2007). Malaria is a leading cause of hemolytic and vaso-occlusive crisis in African children and adolescents with sickle cell disease. Sickle cell disease is the most common inherited hematological disease among Africans. The prevalence of the sickle cell trait (heterozygous inheritance on an abnormal and a normal gene) can be as high as 25–40% in some parts of Africa with 1–3% affected by the disorder (inheritance of a pair of abnormal gene). A paradoxical relationship exists between the sickle cell gene and malaria. The sickle gene is believed to confer some measure of protection against malaria to those with the trait (one abnormal gene); however, it is a leading cause of morbidity and mortality among those with the disorder (two abnormal genes).
Malaria Nephropathy and Splenomegaly
Two other notable chronic effects of malaria in children and adolescents include malarial nephropathy and hyperactive malarial splenomegaly. Malarial nephropathy results from gradual damage of kidney cells by an antigen–antibody complex that is caused by previous malarial infection. There are no reliable data on the magnitude of renal morbidity which are caused by this malaria-induced pathology. However, it is believed that the problem is substantial. Hyperactive malarial splenomegaly (also called tropical splenomegaly syndrome) is another chronic, but less common presentation of malaria among children and adolescents in the tropics. This condition is characterized by an enlarged spleen, high levels of malarial immunoglobulin (IgM), sinusoidal lymphocyte infiltration, and resolution with prolonged antimalarial therapy.
Malaria in Pregnancy
Plasmodium falciparum and P. vivax are known to cause significant effects on maternal and child health during pregnancy. Plasmodium falciparum exerts the worst effects among all the species of malaria parasite. In sub-Saharan Africa, the transmission of P. falciparum is predominantly high and intense with high levels of morbidity and mortality among infants and pregnant women. The major consequences of malaria infection during pregnancy are clinical episodes of malaria, maternal anemia (hemoglobin concentration <11 g/dL), or severe anemia (hemoglobin concentration <8 g/dL), placental parasitemia, intrauterine growth retardation, preterm births, and low birth weight.
Table 12.1 shows the contribution of malaria to adverse maternal and child health outcomes. Malaria in pregnancy is estimated to account for up to 25% of cases of severe anemia, 10–20% of babies born with low birth weight, and 5–10% of neonatal and infant deaths are due to malaria-induced LBW (Greenwood et al. 2005). The effect of malaria in pregnancy is influenced by the level of malaria immunity acquired by the mother before pregnancy. This depends on the pattern and intensity of malaria transmission. The parasite species, the number of previous pregnancies, and the presence of human immunodeficiency virus (HIV) also remarkably impact malaria morbidity and mortality during pregnancy. In areas with high and stable malaria transmission, the prevalence and intensity of P. falciparum parasitemia are higher in pregnant women than in non-pregnant women. The majority of malaria infections in pregnant women living in high transmission areas are asymptomatic because of immunity acquired from repeated exposure to malaria before pregnancy. The adverse consequences of malaria during pregnancy in areas of high transmission are anemia, placental malaria, intrauterine growth retardation, and low birth weight. In areas of low or unstable transmission, acquired malaria immunity is low in all age groups. Pregnant women with malaria in this area are vulnerable to severe manifestation of the disease including cerebral malaria.
HIV and Malaria Co-infection
The evidence that malaria and HIV co-infection increases morbidity associated with both conditions has been confirmed by several studies (Snow et al. 2003). Impact of the complex interaction between malaria and HIV appears to be most profound in pregnancy and children. HIV infection in pregnancy is known to increase the risk of malaria infection (population attributable risk (PAR), 10–27%), maternal anemia (PAR, 12–15%), and low birth weight (PAR, 11–38%) (Steketee et al. 2001). The mechanism by which HIV infection alters malaria morbidity is not well understood. It is believed to be due to systemic and placental immunologic changes that are induced by HIV. In a Rwandan cohort study that included 228 HIV-positive and 229 HIV-negative participants, the incidence of malaria was almost twice as high in the HIV-positive group (6.2 per 100 women-months) than in the HIV- negative group (3.5 per 100 women-months) (Ladner et al. 2002). A review of studies on malaria and HIV co-infection shows that HIV infection in pregnancy significantly increases the risk of peripheral and placental malaria parasitemia. Malaria in pregnant women infected by HIV is more likely to cause higher parasite densities, febrile illness, severe anemia, and low birth weight than malaria in those without HIV infection (Snow et al. 2003). In the absence of HIV infection, the deleterious effects of malaria in pregnancy, notably low birth weight and maternal anemia, were significantly worse in those pregnant for the first or second time than in those who have been pregnant for three or more times (Ter Kuile et al. 2004). With HIV co-infection, the pattern of malaria morbidity is similar across all categories of pregnant women (Ter Kuile et al. 2004).
A review of studies in areas of sub-Saharan Africa with high and stable malaria transmission shows that HIV-1 infection and clinically diagnosed AIDS increased the incidence of malaria 1.2-fold and 2-fold, respectively (Korenromp et al. 2005). In these high transmission areas, HIV-1 infection in children increased hospitalization for malaria and malaria case fatality 6-fold and 9.8-fold, respectively. At the same time in low transmission areas, the incidence of severe malaria and malaria case fatality increased 2.7-fold and 3.6-fold, respectively. The effect of HIV on malaria incidence is worse in HIV patients with lower CD4 counts. In adult patients living in high malaria transmission areas, HIV increased the malaria incidence 1.2-fold, 3-fold, and 5-fold when CD4 counts were ≥500, 200–499, and <200/μL, respectively (Korenromp et al. 2005).
The increase in morbidity and mortality associated with HIV and malaria co-infection, both of which are highly prevalent in most parts of sub-Saharan Africa, calls for more focused research in this area and for integration of service delivery. One way of achieving greater impact is the integration of malaria and HIV/AIDS control activities within maternal and child health programs. Achieving high coverage of insecticide-treated bed nets (ITNs) use and prompt access to treatment with artemisinin-based combination treatments (ACTs) would contribute to the reduction in the morbidity and mortality attributable to HIV co-infection with malaria in high transmission areas. In areas of low intensity and unstable transmission, widespread and effective indoor residual spraying combined with effective treatment using artemisinin-based combination therapy (ACT) is cost-effective and has been shown to significantly reduce malaria morbidity and mortality (Snow et al. 2003).
Strategies for Global Malaria Control
The following section provides a summary of the three-pronged approach to malaria control recommended by the World Health Organization’s malaria control program (WHO 2005).
Vector Control
Indoor residual spraying, environmental management to eliminate mosquito breeding sites, and use of larvicides are known to be effective in reducing malaria when used in combination. Aerial and terrestrial spraying of insecticides is used in parts of South America and Asia to control malaria. This intervention strategy is cost intensive and low in effectiveness. It is therefore, not an appropriate control measure for sub-Saharan Africa given the complex terrains and weak economies of these malaria-endemic countries.
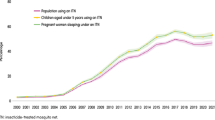
Prevention of Human–Vector Contact
Insecticide-treated bed nets (ITN) have been shown by studies in a variety of settings to be effective in reducing the incidence of clinical malaria by half and fatalities by about a third (Snow et al. 2003). Population coverage for ITN in most parts of Africa remains low (<20%). The low re-treatment rate at the expiration of the usual period of potency (6 months) was a major challenge, even in areas that achieved high ITN coverage. The development and widespread deployment of factory-treated nets with lifelong protective effects (LLINs) has eliminated the need to re-treat insecticide-treated nets. The persisting challenge is how to improve access to ITNs by poor women and children who need to be protected from severe and fatal malaria. The Global Fund for Tuberculosis AIDS and Malaria is providing funding to countries in endemic low and middle-income countries to support this intervention. A systematic review of randomized controlled trials conducted in Africa showed that ITNs used in pregnancy compared to “no nets” significantly reduced the risk of placental malaria in all pregnancies (relative risk 0.79, 95% confidence interval 0.63–0.98). The review also showed that ITNs significantly reduced the risk of low birth weight (relative risk 0.77, 95% CI 0.61–0.98) and fetal loss in the first to fourth pregnancy (relative risk 0.67, 95% CI 0.47–0.97). However, this was not the case in women with more than four previous pregnancies (Gamble et al. 2006). In a large randomized controlled trial in communities with intense and perennial malaria transmission, ITN use significantly reduced the risk of severe malaria anemia, placental malaria, and low birth weight among those pregnant for the first to fourth time, but not in those pregnant for five or more times (Ter Kuile et al. 2003). The adherence to ITN use in pregnancy was shown to be significantly lower in adolescent and young women, who are most at risk for the deleterious consequences of malaria (Browne et al. 2001). This observation and the known risk of higher malaria morbidity associated with first pregnancy (involving mostly adolescent women) make it necessary to specially target this age group for intervention.
In summary, the limited risk assessments undertaken so far with regard to the safety of ITNs suggest that they are relatively safe. However, a cautionary note regarding the need to monitor the health effects of long-term exposure to insecticides in resource-poor settings has been presented by Ehiri et al. (2004). Although the use of mosquito nets is not new, mass use of ITNs as a population-based malaria control tool is a relatively new technology, and some uncertainty remains about the potential for problems as their use expands (Hirsch et al. 2002).
Treatment and Prevention with Drugs
Prompt treatment of malaria with efficacious and affordable antimalarials is a key component of the Global Malaria Control Strategy. The emergence and spread of malaria parasites (especially P. falciparum) resistant to the commonly used affordable antimalarials, like chloroquine (CQ) and sulphadoxine–pyrimethamine (SP), hampered malaria control in Africa and has deteriorated the malaria situation on the continent. The emergence of these multidrug-resistant malaria parasites led to the adoption of combination treatment options as the gold standards for treating malaria. The WHO (2006) recommends that the ideal drug combination should contain two drugs that are individually effective against the blood stages of the parasite and use completely different mechanisms to kill the parasite. Based on results from several well-conducted studies, the WHO recommended that combinations that contain artemisinin (a drug derived from the Chinese plant A. annua L.) or its derivatives and another structurally unrelated and more slowly acting drug provide the best therapeutic effects and are safe. This category of drug combinations is collectively known as artemisinin-based combination treatments (ACTs).
The advantages of artemisinin-based combination treatments (ACTs) have been outlined by the WHO to include the following (WHO 2006):
-
Rapid substantial reduction of parasite biomass
-
Rapid resolution of clinical symptoms
-
Effective action against multidrug-resistant P. falciparum
-
Reduction of gametocyte carriage, which may reduce malaria transmission
-
No parasite resistance documented as yet with the use of artemisinin and its derivatives
-
Few reported adverse clinical effects (note that pre-clinical data on artemisinin derivatives are limited)
Monotherapy with artemisinin derivatives requires multiple doses given for 7 days due to their characteristic short half-life. The other key advantage of artemisinin containing combination treatments (ACTs) is the shortened duration of treatment (3 days), with expected improvement in patient compliance to treatment. If the partner drug is effective, ACTs ensure prompt recovery and high cure rates. They are generally well tolerated. Replacing the older failing or failed monotherapies with effective drugs will reduce morbidity and mortality. The challenge, however, remains how to deliver these drugs to the people that need them. Implementation of this policy would put significant cost burdens on national malaria control programs. However, the costs of failing to change, such as an increase in childhood deaths and high cost of hospitalization, make it a necessary and cost-effective program.
Affordability of ACTs is a major issue affecting their effective deployment in malaria control programs in sub-Saharan Africa. ACTs are generally too expensive for most people in low-income settings where malaria is endemic. While drugs such as chloroquine and sulphadoxine–pyrimethamine (SP), which were previously used for treating uncomplicated malaria, cost only a few US cents, the new ACTs cost about $2–$3.5 and even higher when not discounted. International efforts to address this issue championed by the Roll Back Malaria (RBM) partnership have yielded some positive results, especially through the Global Fund for Tuberculosis, AIDS and Malaria (Brundtland 2002). However, huge gaps still exist. Unfortunately access to prompt treatment with effective antimalarial drugs remains very low in many sub-Saharan countries, leading to the persistence of high malaria mortality rates. The reasons for poor access to treatment are mainly due to weak health systems that are poorly patronized by the populace and a lack of funds to procure and effectively deliver expensive artemisinin-based combination treatment (ACTs). ACTs are necessary since high levels of P. falciparum resistance have rendered chloroquine and sulphadoxine–pyrimethamine ineffective. These were the cheaper treatment options that have been used for several decades. Most children who become ill with malaria in these areas are usually treated at home with poor quality or inappropriately administered medicines that were purchased from local, often untrained drug vendors.
Antimalarial treatment policies, adopted by each country, depend on the epidemiology of the disease, including patterns of transmission, drug resistance, political environment, and economic context. The adoption of ACTs in sub-Saharan Africa was preceded by establishment of local evidence on the effectiveness of existing first- and second-line drugs which have demonstrated consistently high treatment failure rates due to parasite resistance (Snow et al. 2003). The WHO (2006) also recommends that countries developing antimalarial treatment policies should strive to ensure that
-
all populations at risk have access to prompt treatment with safe, good quality, effective, affordable, and acceptable antimalarial drugs and
-
there is rational use of antimalarial drugs in order to prevent the emergence and spread of drug resistance induced by unduly high selection drug pressure on mutant malaria parasites.
Delivery of effective and safe antimalarial treatment to poor rural populations and those in difficult, hard-to-reach settings poses enormous challenges to malaria control programs in Africa. In many endemic countries, the formal health system is weak. Often the health system consists of a few ill-equipped health facilities run by inadequately trained and/or poorly motivated health personnel. The proportion of the people that access these services is so low that successful malaria treatment programs in Africa would be impossible without community-based delivery mechanisms including adequately trained and equipped informal community-based providers and caregivers who provide treatment and preventive services as close as possible to where people live and work. Delivering community health care such as malaria treatment services through primary healthcare centers has long been identified a big challenge by Jeffery (1984) as summarized in Box 12.2. A careful appraisal of these factors in the context of the current situation of malaria control efforts in most endemic countries in sub-Saharan Africa shows situations that are as pertinent today as they were over two decades ago when they were highlighted by Jeffery (1984).
Progress and Challenges of the Global Malaria Control Strategy
The inadequacies of health information systems and vital registration processes in most parts of sub-Saharan Africa make it difficult to obtain reliable records of malaria mortality. Facility-based records of deaths, when available, are not representative of the situation in the larger population given that the majority of sick children do not use health facilities and most deaths occur outside the formal health facilities. Most of the available mortality data from malaria-endemic areas are estimates and prospective mortality data from demographic surveillance systems validated by verbal autopsies (Snow et al. 2004). The inefficiency of health information systems and vital registration processes in sub-Saharan African countries makes it difficult to obtain sufficient and timely information to track the performance of malaria control programs. The malaria situation globally deteriorated in the past three decades. This resulted in increased malaria-related morbidity and mortality, especially in sub-Saharan Africa where emergence and spread of multidrug-resistant malaria parasites and breakdown of malaria control programs were the leading reasons, among others (Korenromp et al. 2003). Greenwood et al. (2005) have given an elaborate summary of the factors believed to have contributed to the deterioration of the global malaria situation in Box 12.3.
Conclusion
The evidence that large-scale and effective use of ITNs can reduce the incidence of malaria and malaria-related deaths is both strong and consistent (Lengeler 2000). Insecticide-treated mosquito nets (ITNs) can reduce all-cause childhood mortality by about a fifth; with about 6 lives saved for every 1,000 preschool children protected with ITN (Lengeler 2000). It is estimated that full ITN coverage in sub-Saharan Africa could prevent 370,000 child deaths per year (Lengeler 2000). Insecticide-treated nets are cost-effective, but endemic poverty and inadequate sensitization of people in malaria-endemic areas remain the major reasons for low use (Snow et al. 2003). The cost-effectiveness of ITNs (US $19–85 per disability-adjusted life year (DALY)) is similar to most childhood vaccines (WHO 2003). When community coverage is high, ITNs not only protect those who sleep under them, but also those in the same dwelling (the home effect) and those living nearby (the community effect) (Snow et al. 2003).
The year 2005 marked the end of the target set by African Heads of State to achieve at least 60% access to prompt and effective treatment of malaria and 60% ITN coverage for under-5 children and pregnant women. However, most countries in sub-Saharan Africa fell far short of these targets. It was also in the same year that RBM set the landmark target of halving malaria mortality by 2010. Appraisal of malaria control efforts at the end of 2005 uniformly indicated that resources available for procurement of malaria control commodities (ACTs, ITN, and diagnostic kits) were grossly inadequate. The appraisal also showed that malaria control personnel at national and regional levels was inadequately equipped.
Donors and governments should develop effective mechanisms to monitor the access that children, adolescents, pregnant women, and children in difficult circumstances have to evidence-based treatment and preventive interventions for malaria. Donor funds specifically tagged to providing resources and infrastructure for effective management of severe and complicated malaria have been grossly inadequate. Supportive care for women and children with severe malaria is grossly impeded by weak health systems in malaria-endemic countries. Funds meant for providing adequate infrastructure and personnel for managing severe malaria should be tagged to bilateral and multilateral health system support grants.
Key Terms
Acquired malaria immunity |
Anemia |
Anopheles funestus |
Anopheles gambiense |
Artemisia annua |
Artemisinin-based combination therapy (ACT) |
Artemisinin-based combination treatments (ACTs) |
Blood transfusion |
Case fatality rate |
Cerebral malaria |
Chloroquine |
Circulatory collapse |
Cortical blindness |
Cytokines |
Dyserythropoeisis |
Dyskinesia |
Entomologic inoculation rate (EIR) |
Fetal loss |
Fever |
Global Malaria Control Strategy |
Glucose-6-phosphate dehydrogenase (G6PD) deficiency |
Hemoglobin |
Hemolytic crisis |
Home management of malaria (HMM) |
Hyperactive malarial splenomegaly |
Hypoglycemia |
Impaired consciousness |
Infant mortality |
Insecticide-treated bed nets (ITNs) |
Integrated management of childhood illnesses (IMCI) |
Intermittent preventive treatment (IPT) |
Intermittent preventive treatment of infants (IPTi) |
Intrauterine growth retardation (IUGR) |
Learning disorders |
Lifelong protective effects (LLINs) |
Low birth weight |
Malaise |
Malaria-endemic countries |
Malaria vaccine |
Malarial nephropathy |
Malariometric indices |
Maternal malaria |
Maternal mortality |
Monotherapy |
Mosquito |
Multidrug-resistant malaria parasites |
Nausea |
Parasite resistance |
Parasitemia |
Perennial malaria |
Placental malaria |
Plasmodium falciparum |
Plasmodium malariae |
Plasmodium ovale |
Plasmodium vivax |
Poor appetite |
Population attributable risk (PAR) |
Poverty |
Pregnancy |
Preterm births |
Relative risk |
Repeated convulsions |
Residual spraying |
Respiratory distress |
Roll Back Malaria (RBM) |
Seizures |
Severe anemia |
Severe malaria |
Sickle cell disease |
Sinusoidal lymphocyte infiltration |
Splenomegaly |
Sporozoite |
Sporozoite rate |
Stable malaria transmission |
Sulphadoxine–pyrimethamine (SP) |
Tropical splenomegaly syndrome |
Uncomplicated malaria |
Under-development |
Vaso-occlusive crisis |
Vector control |
Questions for Discussion
-
1
Globally, women, children, and adolescents in sub-Saharan Africa are known to bear the greatest burden of malaria morbidity and mortality. List any six factors most peculiar to the region that account for this high burden.
-
2
List five consequences of malaria infection in children and pregnant women.
-
3
An integrated approach is advocated as an efficient and cost-effective strategy for the management of malaria co-infection with HIV/AIDS. Briefly discuss what you understand by integrated management and describe how such an integrated approach might be operationalized in practice.
-
4
What are artemisinin-based combination treatments (ACTs) and what are the advantages of their use in the treatment of malaria?
-
5
What are the challenges of community delivery of malaria treatment through existing primary healthcare systems? Is home treatment of malaria a better option? Discuss the reasons for your position.
-
6
List six factors that contribute to the worsening of the global problem of malaria? How can these be addressed? What should be the role of Roll Back Malaria initiative in global malaria control?
References
Breman JG, Alilio MS, Mills A (2004) Conquering the intolerable burden of malaria: what’s new, what’s needed: summary. American Journal of Tropical Medical Hygiene, 71(Suppl 2), 1–15
Briand V, Cottrell G, Massougbodji A (2007) Intermittent preventive treatment for the prevention of malaria during pregnancy in high transmission areas. Malaria Journal, 6, 160
Browne EN, Maude GH, Binka FN (2001) The impact of insecticide-treated bednets on malaria and anemia in pregnancy in Kassena-Nankana district, Ghana: a randomized controlled trial. Tropical Medicine & International Health, 6, 667–676
Brundtland GH (2002) External evaluation of Roll Back Malaria. http://www.rbm.who.int/changeinitiative/externalevaluation.pdf, cited 21 May 2008
Crawley J, Nahlen B (2004) Prevention and treatment of malaria in young African children. Seminars in Pediatric Infectious Diseases, 15(3), 169–180
Ehiri JE, Anyanwu EC, Scarlett HP (2004) Mass use of insecticide-treated bednets in malaria endemic poor countries: public health concerns and remedies. Journal of Public Health Policy, 25(1), 9–22
Gamble C, Ekwaru JP, ter Kuile FO (2006) Insecticide-treated nets for preventing malaria in pregnancy. Cochrane Database of Systematic Reviews, Issue 2
Garner P, Gülmezoglu AM (2006) Drugs for preventing malaria in pregnant women. Cochrane Database of Systematic Reviews, Issue 4
Greenwood BM, Bojang K, Whitty CJM et al. (2005) Malaria. Lancet, 365: 1487–1498
Hirsch B, Gallegos C, Knausenberger W et al. (2002) Programmatic environmental assessment for insecticide-treated materials in USAID activities in sub-Saharan Africa. Agency for International Development (USAID), Office of Sustainable Development. http://www.afr-sd.org/documents/iee/docs/32AFR2_ITM_PEA.doc, cited 16 May 2008
Jeffery GM (1984) The role of chemotherapy in malaria control through primary healthcare: constraints and future prospects. Bulletin of World Health Organization, 62(Suppl.), 49–53
John CC, Sumba PO, Ouma JH (2000) Cytokine responses to Plasmodium falciparum liver-stage antigen 1 vary in rainy and dry seasons in highland Kenya. Infection and Immunity, 68(9), 5198–5204
Korenromp EL, Williams BG, Gouws E (2003) Measurement of trends in childhood malaria mortality in Africa: an assessment of progress toward targets based on verbal autopsy. Lancet Infectious Disease, 3, 349–358
Korenromp EL, Williams BG, de Vlas SJ (2005) Malaria attributable to the HIV-1 epidemic, sub-Saharan Africa. Emerging Infectious Diseases, 11(9), 1410–1419
Ladner JL, Leroy VR, Simonon A (2002) HIV infection, malaria, and pregnancy: a prospective cohort study in Kigali, Rwanda. American Journal of Tropical Medicine and Hygiene, 66(1), 56–60
Lalloo DG, Olukoya P, Olliaro P (2006) Malaria in adolescence: burden of disease, consequences, and opportunities for intervention. Lancet Infectious Disease, 6(12), 780–793
Lengeler C (2000) Insecticide-treated bednets and curtains for preventing malaria. Cochrane Database of Systematic Reviews, 2
Mendie K, Bosman A, Olumese P (2003) Effective delivery methods for malaria treatment. Reducing malaria’s burden: evidence of effectiveness for decision makers. Technical Report Washington: Global Health Council, 39-45
Meremikwu MM, Asindi AA, Ezedinachi ENU (1997) The pattern of neurological sequelae of childhood cerebral malaria among survivors in Calabar, Nigeria. Central African Journal of Medicine, 43, 231–234
Meremikwu MM, Omari AAA, Garner P (2005) Chemoprophylaxis and intermittent treatment for preventing malaria in children. Cochrane Database of Systematic Reviews, Issue 4
Mung’Ala-Odera V, Snow RW, Newton CRJC (2004) The burden of the neuro-cognitive impairment associated with Plasmodium falciparum malaria in sub-Saharan Africa. American Journal of Tropical Medicine and Hygiene, 71(Suppl 2), 64–70
Murphy SC, Breman JG (2001) Gaps in childhood malaria burden in Africa: cerebral malaria, neurological sequelae, anemia, respiratory distress, hypoglycemia, and complications of pregnancy. American Journal of Tropical Medicine and Hygiene, 64(1, 2), S:57–67
Schellenberg D, Menendez C, Kahigwa E et al. (1999) African children with malaria in areas of intense Plasmodium falciparum transmission: features on admission to the hospital and risk factors for death. American Journal of Tropical Medicine and Hygiene, 61(3), 431–438
Snow RW, Craig MH, Newton CRJC (2003) The public health burden of Plasmodium falciparum malaria in Africa: deriving the numbers. Working Paper 11, Disease Control Priorities Project. In: The Disease Control Priorities Project (DCPP) Working Paper Series. Bethesda (Maryland): Fogarty International Center, National Institutes of Health
Snow RW, Korenromp EL, Gouws E (2004) Pediatric mortality in Africa: Plasmodium falciparum malaria as a cause or risk. American Journal of Tropical Medicine and Hygiene, 71(Suppl 2), 16–24
Steketee RW, Nahlen BL, Parise ME (2001) The burden of malaria in pregnancy in malaria-endemic areas. American Journal of Tropical Medicine and Hygiene, 64(1,2), S: 28–35
Ter Kuile FO, Terlouw DJ, Phillips-Howard PA et al. (2003) Reduction of malaria during pregnancy by permethrin-treated bed nets in an area of intense perennial malaria transmission in western Kenya. American Journal of Tropical Medicine and Hygiene, 68(Suppl 4), 50–60
Ter Kuile FO, Parise ME, Verhoeff FH et al. (2004) The burden of co-infection with human immunodeficiency virus type 1 and malaria in pregnant women in sub-Saharan Africa. American Journal of Tropical Medicine and Hygiene, 71(Suppl 2), 41–54
Vallely A, Vallely, L, Changalucha J et al. (2007) Intermittent preventive treatment for malaria in pregnancy in Africa: what’s new, what’s needed. Malaria Journal, 6:16
World Health Organization (1992) Ministerial Conference on Malaria. Amsterdam Netherlands 26–27 October. WHO CTD/MCM/92.3
World Health Organization (2003) Cost-effectiveness of social marketing of insecticide-treated nets for malaria control in the United Republic of Tanzania. Bulletin of the World Health Organization, 81(4), 269–276
World Health Organization (2004) A strategic framework for malaria prevention and control during pregnancy in the African Region. WHO Document: AFR/MAL/04/01. Brazzaville: World Health Organization Regional Office for Africa
World Health Organization (2005) World Malaria Report. Geneva: World Health Organization. http://www.rbm.who.int/wmr2005/html/map1.htm, cited 15 May 2008
World Health Organization (2006) Guidelines for the treatment of malaria. WHO/HTM/MAL/2006.1108. Geneva: World Health Organizagtion. Cited August 8, 2009
World Health Organization (2007) International travel and health: situation as of 1 January 2007. Geneva, World Health Organization. http://whqlibdoc.who.int/publications/2007/9789241580397, cited 21 May 2008
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2009 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Meremikwu, M., Ezedinachi, E., Ehiri, J.E. (2009). Malaria in Women and Children. In: Ehiri, J. (eds) Maternal and Child Health. Springer, Boston, MA. https://doi.org/10.1007/b106524_12
Download citation
DOI: https://doi.org/10.1007/b106524_12
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-0-387-89244-3
Online ISBN: 978-0-387-89245-0
eBook Packages: MedicineMedicine (R0)